The following is a lightly edited version of a patient testimonial I wrote in December 2014. I wrote it to include as a required element of a letter of intent package for a research network funding application to the Canadian Institutes of Health Research Strategy for Patient-Oriented Research.
At the time, I emphasized to the principal investigators (PIs) that I recommended finding a patient partner uncomplicated by the duality of being both a patient and a scientist. I know that my experience as a patient is no longer typical, and I knew some reviewers would criticize that. But the PIs wanted this, so this is what I provided. It hurt–in a way that grant reviews don’t usually hurt–to read assessments of my testimonial. One reviewer was concerned that I was not an “authentic” patient. But we still got through the letter of intent stage and the network was ultimately funded. One of my roles in the network is to serve as a patient-researcher bridge. It’s a service role for me, except instead of being service simply to an academic community, it’s also service to the community of people in Canada whose lives are affected by diabetes.
I’m sharing this here now for some complicated reasons. One of the reasons is that the research network will have a meeting soon at which we will be asking people to share their own stories, and I feel hypocritical given I haven’t shared mine very openly. I’m also doing it because I had tests this winter due to some alarming symptoms and then waited … and waited … for results I received recently. Everything is fine. I’m beyond relieved, but now all the fear I had been holding at bay for days and weeks and months is washing over me. I’m shaken up, and I’ve come back to this testimonial to reflect on how I navigate waves of fear. Finally, and perhaps most importantly, I’m sharing for a friend who knows who they are.
—————————–
I was diagnosed with type 1 diabetes – or juvenile diabetes, as it was called at the time – in January of 1983 in Regina, Saskatchewan, shortly after I turned 7 years old. I spent the following month in Pasqua Hospital, learning to pinch up the skin of an orange to inject a needle, and playing with the other kids in the ward. I especially loved playing with a younger child down the hall, who was hospitalized with leukemia. She wasn’t talking much yet and I was one of the few people who seemed to entertain her. Under the nurses’ supervision, I was allowed to take her to play in the playroom. One day, she wasn’t in her room anymore. At 7 years old, I internalized the message: diabetes meant needles and eating everything on my plate, nothing more or less, but at least it wasn’t leukemia.
Eventually, I got to go home and, to my joy, go back to school. I adapted to life with diabetes, and it faded in importance as other life issues took prominence. My parents gave up yelling at each other and divorced, my dad moved overseas, my mom became involved with an abusive man, and, over years, my family spiraled down into financial insecurity as my mom slowly relinquished her income, our family savings, and her self-esteem. My health was not my primary concern. As a teenager, I got part-time jobs in a local drugstore and a telephone survey company, which meant that I could buy groceries and get our phone back on. I figured out that I could save money and lose weight effortlessly by taking less insulin. My dad was seven provinces and an ocean away; my mom was depressed and unemployed. I no longer had an adult going to medical appointments with me, so I mostly stopped going. After all, it wasn’t as if I had something serious like leukemia. When we moved provinces, my mom didn’t arrange a new diabetes care team. Instead, she asked me why I ‘chose’ to develop an autoimmune disease and encouraged me to repeat a mantra about the sweetness of life.
I made it through those years. I got scholarships and completed an undergrad degree at Queen’s University in Mathematics and Engineering, still with suboptimal health habits. I don’t know what my Hemoglobin A1c was during that time. I had no regular doctor. I could get prescriptions for insulin and test strips at the student health clinic. I took slow-acting insulin every day and fast-acting at meals, doing my best on my own to get the amounts and their timing right. I studied, played sports, and got involved in extracurricular activities. I was not well, but I got by. I didn’t know any better, and I didn’t realize until years later how dangerous some of my actions were. One year, I caught a stomach bug. I hadn’t been sick like that in a decade, and I mistakenly thought that the fact that I wasn’t eating meant that I shouldn’t take any insulin. I ended up in Kingston General in acute diabetic ketoacidosis. The attending diabetes specialist learned that I didn’t have a physician following me, and offered to take me on in his practice. I didn’t understand his concern. In my mind, it was still not serious. After all, it wasn’t leukemia, and my parents had never shown concern about me having a diabetes specialist or not.
In between events like those that horrify me now in retrospect, I did my best to have what I thought was a normal life. I dropped out of undergrad for a year to make money and get a change of scenery. I worked at a manufacturing plant, then took a job cooking on a charter sailboat in the Bahamas. (I wasn’t even very familiar with oceans and had zero sailing experience, so it was a change of scenery, alright.) I came back, graduated from university, lived in Bolivia where I volunteered with a women’s organization, and then came back to Canada again and started working full time as an engineer at the plant where I had previously worked. For the first time in over a decade, I had a regular routine, and I started to get a handle on what it meant to take care of myself. A few years later, when I started graduate school in Human Factors Engineering at the University of Toronto, I finally had access to primary care through the student health service. When I got funding to work on a project in health informatics, one of the clinicians on the team connected me with an endocrinologist at St. Michael’s Hospital in Toronto who was accepting new patients.
The further along I went, in life and in school, the better I was able to live with diabetes. Just having proper access to health care was a big improvement for me, and new technology kept coming out and revolutionizing my life. Shortly before I got married, I got my first insulin pump and, for the first time in my life, was able to calibrate my basal insulin delivery to my body’s pattern of basal insulin needs. When I was finally able to achieve relatively stable blood sugars for the first time in decades, my energy level went up incredibly. I told my husband, “If this is what non-diabetic people feel like all the time, they should be doing more with their lives!”
During my years in graduate school, I developed hypoglycemia unawareness, meaning that I could no longer easily feel when my blood sugar was low. My blood sugar started dropping dangerously low in increasingly unfavourable conditions, like a 3-hour morning class in the Centre for Global eHealth Innovation into which I was not allowed to bring any food, not even for medical reasons. I stepped out of that class so many times to treat a low, and to cry. Then, one day during my postdoc when I was traveling alone, I uncharacteristically failed to show up to a morning meeting. My postdoc mentor called 911 and I was brought to consciousness by emergency responders. I got my first continuous glucose monitor after that event, a Dexcom 7+. Dex, as that beloved device was known in my family, significantly increased my quality of life, and made my second healthy pregnancy feasible even as I was living the chaotic life of a traveling postdoc, going back and forth between my fellowship at the University of Michigan, and my family in Toronto.
When people ask, I usually tell them all those good things. I talk enthusiastically about how technology like better insulins, insulin pumps, and continuous glucose monitors have allowed me to have healthy pregnancies and now to juggle my roles as a tenure-track professor, a mother of two, and a person living with chronic disease. I tell them about promising technological advances on the horizon. In other words, I put on my optimistic face. After all, it isn’t leukemia.
I am far less open about how scared I am that my past has screwed up my future. Five years ago, I had routine annual lab work done. My primary care provider called me in to give me the news that my urinalysis was showing kidney damage. I thought my childhood and teenage years had finally caught up with me, and I was devastated. While waiting to see my endocrinologist to find out more, I kept my devastation to myself. I don’t like to hurt in front of others; I saw what being vulnerable did to my mom. When I got the bad news, it was May in Toronto, that time of year when the magnolia trees start to bud and the brown of winter is washed away. One warm afternoon, I walked my then 3-year-old son home from daycare as usual. He ran ahead of me in that beautiful, joyful way that children do, bounding along in the spring sunlight. I saw the movie trope, where the child runs along, growing into an adult frame by frame, and I thought, “I will not be here to see him grow up.” That belief blanketed my skin in those weeks, like a layer of cold, numbing everything else. When I finally saw my endocrinologist, she told me that the test had a high false positive rate and she wouldn’t even start to worry unless I had two positive tests. She also explained that my long bike ride less than 12 hours before the test could easily have caused its result. My second test was negative, and I breathed again, but my breath wasn’t forceful enough to blow away the thin layer of fear that clings to me to this day.
I led a study a few years ago testing ways of dynamically visualizing risk to help people understand randomness in health risk. I used cardiovascular risk as the study context with a Framingham model on the back end. While developing the interface for the visualization and getting the study ready to launch, I tested aspects of the interface repeatedly, sometimes clicking ‘yes’ to diabetes, other times ‘no’. With those repeated visualizations, I literally saw the impact of diabetes as a risk factor. It was not heartening. My primary care doc reassuringly pointed out last time I saw him that my blood pressure is excellent and, “You have the lipids of an Olympian. I wish mine were that good.” And yet, I worry about all the microvascular and macrovascular damage that might have happened when I was young and lacked appropriate support. Every time I have blood work or urinalysis done, even though intellectually I know that my chances of receiving a clean bill of health are very good, I fight my anxiety as I await the results.
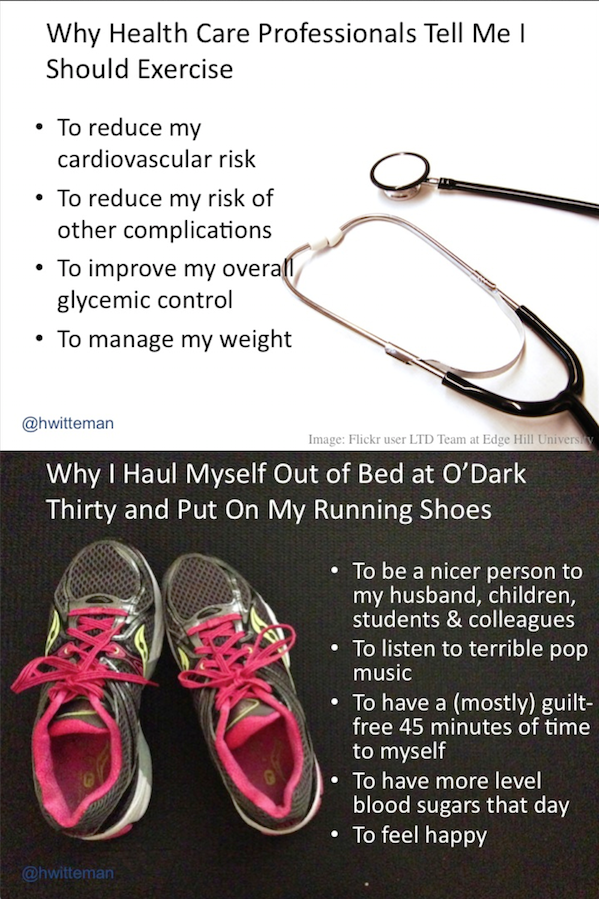
The deadline for this letter of intent is near my 32nd ‘diaversary,’ the term used in the diabetes community to refer to the anniversary of one’s diabetes diagnosis. I’ve lived a lot longer than my young friend with leukemia. I am grateful. I wish she could have had the same opportunities I’ve had. But I realize now that diabetes has a seriousness all its own. Partly out of a desire to compensate for my early years, I maintain tight control and tediously healthy habits. I walk the constant fine balance between the low blood glucose that could kill me quickly and the high blood glucose that could kill me slowly after first significantly decreasing my quality of life. Working so hard to maintain impeccable control means that diabetes looms large in my life. It affects my life in a multitude of ways and interferes with my plans and activities on a daily basis. I know that my years of good control as an adult are putting me in a good position to be here to raise my children, have a successful career, and hopefully do some good in the world, but I can’t unfeel my fear. My entire conscious life, I’ve been reminded–in doctor’s offices, scientific articles, news items, conference presentations–that I am at risk. In ‘Taming the Tiger, Your First Year with Diabetes,’ William Dubois writes, “Can you have a pet tiger? Sure. As long as you feed it well, groom it, and never turn your back on it, you can co-exist with a tiger in your living room. But if you neglect the tiger, starve it, turn your back on it–the tiger will pounce on you and tear you to shreds.” I worry that the tiger is harbouring resentment about the years my parents and I neglected it.
When I was invited to be a part of this project, I gave it more careful thought than I give most requests to collaborate. As with any project, I considered the time commitment. As a tenure-track professor with a young family and a time-consuming chronic disease, I am very disciplined about managing my workload. I have my own emerging, successful research program, and I need to care for it. I also thought hard about the difficulty of wearing my researcher and patient hats simultaneously, and whether it’s good or fair for me to take this role. I am active and engaged in the diabetes community and have a number of friends who also live with diabetes. Hearing other peoples’ stories keeps me aware that my experiences as a patient are no longer typical. I have lived the shift from decades of being a patient to now being a patient/colleague, and the change has been marked. I will always remember an intake appointment with a maternal fetal medicine specialist when I was pregnant with my second child. As the interview went on, it became clear that the specialist wasn’t really listening to me when I mentioned some particularities about my body and my life. I became frustrated with the dynamic in the room, so when we got to the question about what I did for a living, rather than giving the usual vague answer like, “student,” or, “postdoc,” I pulled out all the stops: “I’m a postdoctoral fellow in Internal Medicine at the University of Michigan.” The entire tenor of the conversation changed. Suddenly I was a person worth listening to, not just a body to be treated. I shouldn’t have to say that to be taken seriously.
In the end, I agreed to participate in this project because although I desperately want the research and clinical communities to already be at the point where all patients are listened to, not just those who have advanced training, I am acutely aware that we are not there yet. As a patient and also as a researcher in this area (e.g., I am PI of what is thus far the only project outside the United States funded by the Patient-Centered Outcomes Research Institute), I see this in my conversations with fellow researchers, even those who have the very best of intentions. After giving it a great deal of thought about what roles I can–and should–play, I finally agreed with the conclusions of the scientists who invited me to participate on this proposal: one of the uniquely valuable ways I can help move health research in Canada toward the goal of being truly patient-oriented is to make use of the fact that I am a scientist who also happens to have over three decades of experience of living with diabetes and the very real personal fear of complications. With this rare dual background, I am equipped to provide skilled translation between patient and researcher points of view. I have been involved in the development of this proposal and have provided many comments and suggestions from my dual perspectives, including as a person with diabetes. I am committed to using my expertise to help scientists learn how to work with patient partners and keep their focus on the people living with the disease. I am also committed to mentoring other patient partners within this project and using my network of personal contacts to help recruit new patient partners. In short, I will use every tool in my toolbox to ensure that all of the research undertaken within this proposed network reflects the diverse priorities and perspectives of people living with diabetes in Canada.

3 thoughts on “Patient Testimonial”
As a parent of a newly diagnosed type 1 diabetes manager, I can’t tell you how much I appreciate this post. My son is 10 coma and I constantly emphasize to him how important taking care of himself is now, and how it pays off in the future. I live in fear everyday, not only for the issues that arise on a day-to-day basis, but for what the future holds. How does a 20-something in an entry-level job afford insulin? Especially when they are hustling to get ahead and make ends meet, it gets put on the back burner. Terrifying.