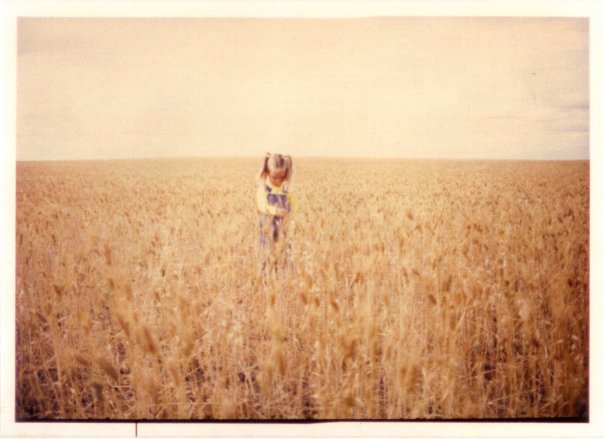
Me, a few years pre-diagnosis:
I was diagnosed with diabetes 33 years ago yesterday. I spent a month living in Pasqua Hospital in Regina, Saskatchewan, injecting insulin into an orange, making friends with a little girl with leukemia, and missing school desperately. When I went home, I took Toronto & NPH insulin twice a day and also tested my urine twice a day in test tubes with tablets that fizzed and changed colour.
After about 20 years of living with diabetes, I started noting the day of my annual diaversary (anniversary of diagnosis). I don’t throw a party, but I acknowledge the day to myself. When I was a kid, life expectancy for people with diabetes was not as good as it is now, and I still remember the note of doubt in the doctor’s voice answering my mom’s question about whether I would ever be able to have children. (And then, a few years later, Steel Magnolias happened.) So each year now, I celebrate a little bit that I’m alive, a mother of two, with no end organ damage. This latter point is more likely due to luck than anything else, though I think I’ve done an OK job since reaching adulthood of managing diabetes well.
This year, I’m sharing some of the things I’ve learned in those decades — about diabetes, and about myself — in case they might be helpful to others. As always, YDMV (your diabetes may vary).
1. Overall, I’ve found that I get better at it as I go on, but it also gets more tiring and harder as my life gets busier while I run out of important hormones.
2. As a person with type 1, if I try to distance myself from the stigma of type 2 by emphasizing the differences between types, I may contribute to the exact stigma I am trying to avoid.
3. Many nutritional information sheets are wrong. Some of them are really wrong. (Looking at you, Ace Baguettes.) I measure and calculate, but I always keep in the back of my head that even if I calculate correctly based on the numbers they give me, those numbers may be wrong.
4. My meter reading may be wrong, too. Readings are allowed to vary by +/- 15% or 20% and that’s if the meter and strips are within guidelines, which they may not be. My meter may be totally off.
5. Even if I do everything right, my BGs (blood glucose, or blood sugars) may be off. Even if I do everything right, I may develop complications. When something goes wrong, it doesn’t mean that I’ve done anything wrong or that I am a Bad Diabetic. There are a lot of variables in this system and I only have a say over some of them. As a generally high-achieving person, making peace with this has been critical to my well-being.
6. If I eat fewer carbs, there is more room for error in carb-counting. I am not advocating low carb. Full respect to those doing Type 1 Grit, but I choose to direct my capacity for intensity in other directions. (*cough*grants*studies*papers*cough*) However, I do keep in mind that it’s easier to recover from smaller errors. If one cracker is listed at 3 g CHO but it’s actually 2.6 g, the 1.2 g error associated with bolusing for 3 crackers is not a huge difference whereas the 4.8 g error associated with bolusing for 12 crackers starts to get significant. The first gives me ~0.1U insulin more than I need, which will drop me ~0.3 mmol/L or 6 mg/dl — no big deal. But the second error gives me ~0.4U insulin extra, which will drop me ~1.2 mmol/L (22 mg/dl) — that’s a big deal when I’m maintaining tight control.
7. I have three data points: my continuous glucose monitor (CGM), my meter, and how I feel. If two of them agree, that’s probably what’s going on.
8. Hypos (low blood sugar) are hilarious until they suck the fun right out of everything.
9. About a year after my second child was born, I realized that I find it helpful to think of diabetes sort of like my third child. It takes up about that much time. And every workday is bring-your-diabetes-to-work day! Sometimes it throws a temper tantrum in the middle of a meeting, or, on one memorable occasion, a job interview. I find this a useful analogy when trying to explain what living with chronic disease means to people who don’t have personal experience, but who do have children.
10. Despite useful analogies (see point 9), it’s hard for people who don’t live with a chronic disease or other similar challenges that have no end in sight to truly understand the never-endingness of a health condition that requires so much vigilance.
11. There is a difference between endurance activities and power activities. Once I understood this critical difference, planning for exercise became so much easier. (This book helped me a lot when I briefly played sports at the national level.)
12. Exercising first thing in the morning before eating requires way less planning than at any other time of day. I am not a natural morning person. I did not enjoy learning this.
13. I find it really hard to advocate for myself, but I need to suck it up for myself and for the others who will come after me. I will always remember the class I took during graduate school where I was not allowed to bring in any food to treat hypos because, I was told, of electronics running beneath the floors. It was a 3-hour class right after a meal and I was dealing with fluctuating insulin needs and new hypo unawareness. I had to step out of class so many times to treat a hypo, and to cry. As a university professor now, I hope desperately that I will never inadvertently put a student in a position like that. I wish I had been more confident at the time and contacted student services. I try to do a better job now. For example, when a medical resident used terrible communication methods not long ago, I took a deep breath, thought of their future patients, and offered some feedback.
Special note: This isn’t a personal learning, but speaking of advocacy, it’s almost February 1. That means it’s almost time for the annual 2-week campaign Spare A Rose in which people forgo one flower (or more) for Valentine’s Day and donate the difference to the International Diabetes Federation’s Life for a Child program to provide life-saving insulin to children in developing countries. As Kerri puts it so eloquently: Flowers die. Children shouldn’t. Please consider participating in and promoting this life-saving campaign.
14. There are people out there who, when you have a major hypo on one of your early dates, deal with it like a champ. (I married him.) Having a partner who participates in diabetes care is an incredible gift.
15. Having a pregnancy with diabetes is like taking an unpaid internship as an appointment attender. I kept count at the end of my first pregnancy: I was spending 16 hours a week total traveling to appointments, waiting in waiting rooms, being in appointments, and traveling back. I was in grad school at the time and had the flexibility for this. I have no idea how I would have done it otherwise. For my second pregnancy I saw a less intense team, but it was still a major time commitment.
16. Breastfeeding an infant and a backcountry hiking trip use the same basal pattern for me: roughly 60% of normal basal. Having refined that basal pattern on pre-parenthood hiking trips really came in handy when I had babies. With nursing toddlers (= less predictable & less frequent nursing) I found that a regular basal pattern worked well but I needed to turn on a 1 hour zero basal each time I nursed him. Otherwise, without fail, I would bottom out about 2-3 hours after nursing.
Hiking basal pattern works great for this:

Let’s not talk about the challenges of combining the two:

17. With a supportive health care team and some luck, it is possible to have a fairly straightforward birth with diabetes. My second child was born by uncomplicated, spontaneous VBAC at 41 weeks, which pleased my easygoing maternal-fetal medicine doc, and horrified the nurse on duty when I arrived at the hospital already complete & pushing. One of the things that I suspect may have helped was that I continued to exercise at least an hour a day during that pregnancy, including showing up to appointments on my bicycle. I will always remember that I biked to the hospital for a biophysical profile on a Wednesday and early Friday morning I was back (in a vehicle this time) to have the baby.
18. Clipping my pump on my boot is a great way to avoid annoying tugging at my skirt waistband. I wear a lot of skirts with boots for work, so this is a small change that has really made a difference for me. The only problem is at airports when I have to take my boots off and thread the pump back up under my skirt. It is, uh, not graceful.
19. Traveling with diabetes is tough. Not impossible, but tough. Maintaining the same level of control while in unfamiliar circumstances ramps up the level of difficulty. I often end up restricting what I eat when I travel, which is a bummer, because there go many of the pleasures of travel, but I dislike passing out more than I like exciting food.
20. I need to always bring a spare pump when traveling and never, ever, EVER pack extra diabetes supplies in checked baggage. I learned this the hard way when visiting my husband’s relatives in Antigua, where flights from Canada are infrequent enough that if they lose your bags, even if they find them, you won’t be seeing them for up to a week.
21. Related to the above, Tom Bihn bags are excellent. Since my husband splashed out and gave me an Aeronaut 45 for my birthday the year I started a postdoctoral fellowship that required 30 trips in 2 years, I have traveled extensively for work and fun without ever checking luggage. I can fit a full week’s worth of conference wear, running gear, pump/hypo/other supplies, and multiple pairs of shoes in a carry-on. It is my Mary Poppins bag.
22. Getting super excited about each new cool thing coming out of research is a recipe for disappointment. When I was a child and I saw news items about how a new finding might lead to a cure for diabetes in as little as 5-10 years, I honestly believed them. Thirty-three years later, I am much less excitable. Call me when something works in humans. (But I confess that I can’t help but get a little excited about human trials. Looking at you, ViaCyte.)
23. Makers of diabetes tech apparently either don’t think it’s important to go outside, don’t live places where it gets cold, or simply can’t overcome the challenge of making electronics work in cold weather. I like snowshoeing, skiing, and winter camping, and it’s such a huge pain to have to keep my insulin, tubing, and test meter touching my body at all times so they don’t freeze. The hate in my love-hate relationship with diabetes technology comes from issues like this.
24. When people want to tell me about their grandmother with diabetes who lost a foot, I can choose to assume that rather than trying to scare me, they are trying to connect with me about an issue that affects us both in some way. They are showing that they care about diabetes, and, by extension, about me.
25. If I had to choose between a pump and CGM, I would take the CGM. The value of the CGM is not just in the first-order data (estimates of my current blood glucose). It’s in the second-order data (estimates of whether my blood glucose is stable, climbing, or falling). The arrows & patterns give me invaluable information. Having a CGM has allowed me to fine-tune my basal rates, find a weekday breakfast that gives me rock-solid flat blood sugar (full fat plain yogurt with nuts, seeds & some raisins = 16.5 g CHO), develop techniques that work with my body to blunt spikes in blood sugar (e.g., bolusing ahead by 30-40 minutes when I’m going to have something that is high in carbohydrates and low in fat & protein) and, most importantly, has allowed me to manage my hypoglycemia unawareness. Combining the CGM with xDrip gives me an extra layer of safety when I am traveling solo. xDrip is a DIY system developed by people with diabetes and parents of children with diabetes that pulls data directly from my transmitter, processes it, sends it to a cloud server, and allows my husband to see my data and get alerts even when I am halfway around the world. This is important to me because 6 years ago, before I had a CGM, I had a severe overnight hypo while traveling alone that required paramedic help. The paramedics only came because I had a caring colleague who noted that I hadn’t shown up to a morning meeting, and that was extremely unlike me. She contacted my husband to get the address of where I was staying and then called 911.
26. In my opinion, Minimed makes a better pump than Animas, but the Dexcom sensor is light years ahead of Enlite. Dexcom has better insertion, better accuracy and lasts me 3 weeks versus the 5-6 days I got with the “new” Enlite when I gave it a 3 month trial.
Minimed: Your sensor requires 18 steps of directions (not exaggerating) to insert properly, 2 of which are extremely prone to failure. It also has a very finicky calibration routine. This means it is just not workable in the life of a normal human being. I’m sure it performs well enough in efficacy trials but I predict problems when you hit the effectiveness stage and have to deal with real humans, not just those who are motivated enough to join your trial and adhere to strict intervention fidelity requirements.
Animas: Update your pump design. How many years has it been? It is painful to me, as a human factors engineer and as a person who uses modern technology, to use your pump with its 2-seconds-per-screen-change and terrible menu structure. Also: “Vibe”? Seriously, who names these things? (Or, more disturbingly, what do you do with these during testing?)
Dexcom: I don’t need the y-axis to go to 22.5. You’re validating on every screen change anyway, why not allow a responsive (or better yet, user-set) scale?
27. High blood sugar provides an interesting buzz. When I was a teenager and spent a lot of time with high BG, it made me feel very mellow, which was a welcome emotion at a time of much instability in my family. It also saved money during a time when money was scarce and helped me avoiding gaining weight. (Win-win-win! Or so I thought at the time. Sigh.) I have mentioned this to clinicians and clinician-researchers and I confess I’ve always been a little dismayed at how few of them had ever thought about issues beyond the stereotype of a rebellious teen. (Once again emphasizing the importance of patient-partnered research.)
28. I am probably never going to react well when a nurse at a diabetes clinic extends their hand, expecting me to casually drop my pancreas pump into it. (Nurses/CDEs: Please ask me. Ideally, say please. Recognize that this device keeps me alive and I’ve met you maybe twice. Handing it over is not a neutral thing for me.)
29. I shouldn’t have let my kids try glucose tabs. I have never treated a hypo in peace since.
30. One of the dubious milestones of parenting with diabetes: Noticing the developmental stage at which your children are speaking clearly enough that they can be trained to call 911. In our drill, I pretend to be the operator: “9-1-1, what’s your emergency?” and my kids are trained to respond, “My mommy is sick.”
31. “Adherence” doesn’t mean anything different than “compliance” when the attitudes underlying the words haven’t changed.
32. In 33 years, I’ve had 4 very scary diabetes-related events. Three severe hypos that required help from emergency medical services, and one false positive complication. It’s only 4 events over 33 years, but 4 is more than zero. It’s incredibly irritating to have people suggest that I shouldn’t worry. It is not comforting. My worries are legitimate. They are grounded in real risks, and real events that I have already experienced. Being worried helps me take care of myself. Once I understood this and decided that my feelings were more valid than other people’s ideas of how I should feel, it got much easier to deal with those kinds of comments. Having said that, striving for perfection is a recipe for anxiety for me.
33. There are things that I understand intuitively that I don’t know if I could understand if I didn’t live with something as constant as diabetes. I am a scientist and I do research in health informatics for health education, communication & decision making. My research is broader than diabetes, but having already lived as a person with chronic disease for decades before I became a scientist has offered me many insights that I’ve used in my work. If I could give this gift of insight back, I probably would, but I lost the receipt.
Bonus point. I am a professor, a mom, and I have a time-consuming chronic disease. I am a better professor and a better mom when I’m in good health. Although it often feels like these 3 things are competing for my limited time and focus, I try to keep in mind that taking care of my health is an investment in being able to continue to do the things about which I care deeply: care for my family, and do work that I love. This is easier to write than it is to do. When I am woken to an alarm from my CGM because the designers can’t seem to understand that perhaps it would be a good idea to have different settings at different times of the day, I rarely think, chirpily, “This is an investment in my future!” But doing my best to keep this in mind helps me keep the pieces of my life, seemingly in tension, integrated into a coherent whole.

