In January of this year, I reached 40 years of living with type 1 diabetes (T1D). Over that time, I’ve learned a lot about managing T1D and have been able to get results that satisfy me for some years now. What that means in numbers for the folks who want numbers (skip to the next paragraph if you don’t care to read numbers or don’t know what these things mean): my A1c in % is typically in the mid-5’s. My last two A1c’s were 5.5% or 37 mmol/mol. My 90-day time in range using the international standard 3.9-10 mmol/L (70-180 mg/dl) is typically around 90-92% in range, with the remainder evenly split between low and high. My 90-day standard deviation floats between 1.6-1.9 mmol/L (29-34 mg/dl) and my coefficient of variation is always below 36% and often below 30%. I strive for 0% low but spend a fair amount of time steadily coasting along at 3.7-3.8 mmol/L or 67-68 mg/dl, and I know that nondiabetic people run flat at those numbers, too. My real lows are usually mistakes on my part about when food would be ready or how my body would digest it. My time spent high is usually due to site problems, mistakes on my part about how a food will hit, and me being too slow to get all my winter gear on and get out the door after I’ve deliberately underbolused prior to exercise.
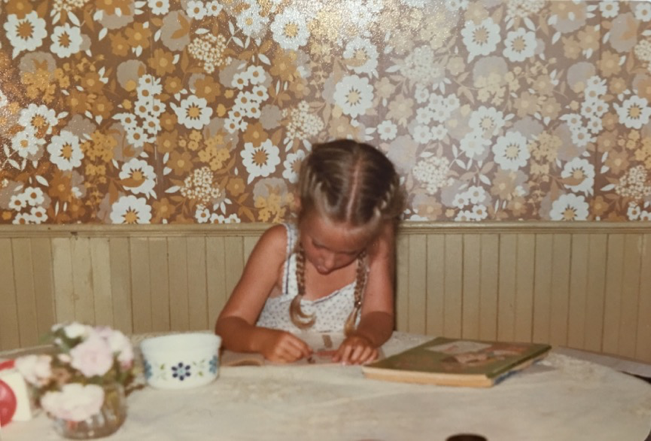
My childhood management was not as good. I had a lot of severe hypos as a child and became way too familiar with the feeling of coming to consciousness and vomiting post-glucagon. Then, from too early an age, my T1D management was left up to me, with insufficient parental oversight. After our mom left our dad and our dad moved overseas, my younger sister and I would often get our own groceries and meals. I have memories of eating cereal for all my meals and going to medical appointments on my own, if I went at all. For a while during my teens, I was the only person in the house with a job. When my mom, sister and I moved thousands of kilometres away to a new city in a new province during my teen years, my mom did not transfer my care to a new diabetes care team. She did, however, ask me why I “chose” to have diabetes and encourage me to repeat mantras about, “the sweetness of life.” This, to say the least, was not a great substitute for seeing an endo or diabetes educator. I went years without ever seeing getting any diabetes-specific care. I had a family doctor who would write prescriptions for the same old insulin, but never reviewed my records, updated my insulin, nor ensured I saw anyone with more diabetes knowledge. As I got older, I moved on and focused on doing the best I could as an adult, but that’s the reality of my history. The further I get from that history, the more I can see how it shaped my feelings and goals about T1D and the rest of my life.
I don’t always do much for my anniversary of diagnosis, or diaversary. Seven years ago, I made a list of 33 things I’d learned in 33 years with T1D. This year, I decided to write a longer post that required more time to reflect, distill, and write about management-focused lessons I’ve learned over the years. I wrote this over the course of many months. I initially thought I would post it on my diaversary, but I wasn’t anywhere near done! I kept poking away at it as I could find bits of time to reflect and write, so here it is, finally, after about six months of writing a paragraph or two whenever I had time. (Hopefully all the links still work.)
Below are some of my reflections and lessons learned about managing T1D for 4 decades. I present them here alphabetically by category, in the hopes that they might prove useful to at least one other person with T1D out there. I have gotten so much useful how-to information from fellow T1Ds, and I always aim to share my own useful information when I can. Please feel free to take and share anything that works for you, and leave the rest.
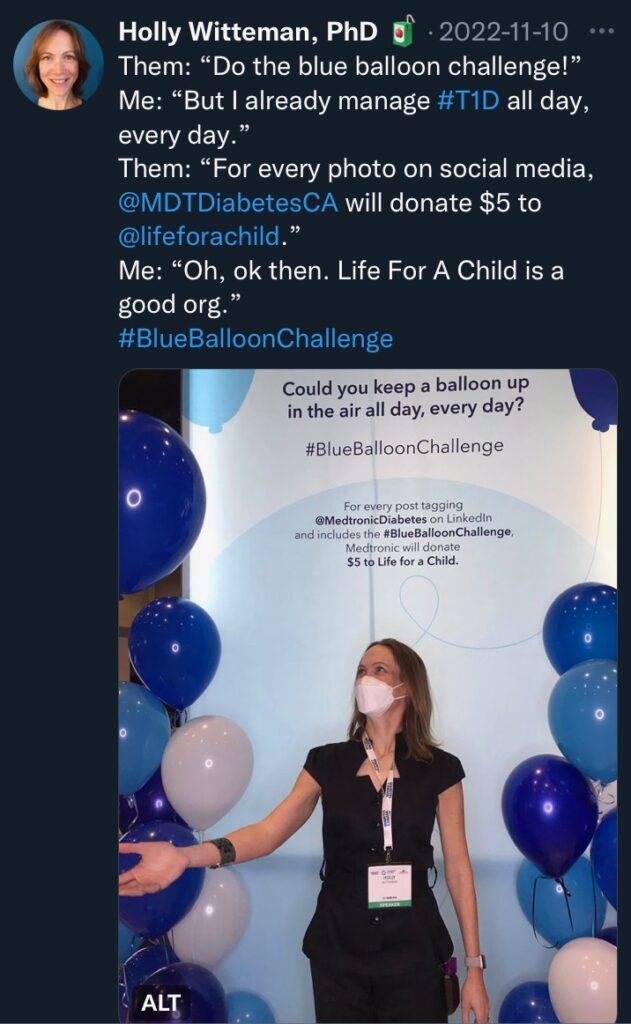
Note to those without T1D (can we call you pancreatypicals?): this is not a 101-level post. It’s written for others managing T1D (their own or someone else’s) who already understand terms. If you care about people with T1D and can manage it, please consider donating to organizations like T1International, Life For A Child, and JDRF, and please support legislative efforts where you live to make diabetes management tools (medication, technology, education, care, support) available to everyone who needs them. If you are new to T1D and don’t know some of these terms, I recommend the Juicebox podcast Defining Diabetes series.
Topics:
- 10 Most Valuable Lessons
- Attitudes & Beliefs
- Backcountry Camping
- Biggest Bang for the Buck
- Burnout
- Comfort In, Dump Out
- Complications
- Consistency
- Control
- Daily Kit
- Data & Reports
- Energy Up Front
- Fibre
- Finances & Insurance
- Highs & Spikes
- Hypos
- Insulin
- Logging Food
- Looping
- Matching Insulin & Food
- Mental Health & Stress Management
- Oops
- Outdoors
- Parenting
- Perimenopause
- Physical Activity (Exercise)
- Physical Activity (Exercise) with Insulin on Board (IOB)
- Podcasts
- Prebolusing
- Pregnancy & Breastfeeding
- Protein & Fat
- Repeated Foods
- Rollercoaster, Get Off The
- Routines & Rituals
- Science & Research
- Settings, Having A Record Of
- Sleep
- Support
- Technology & Tools
- Travel
- Water
- Weighing Food
- Weight Management
- Zealots
- Thank you
10 Most Valuable Lessons
Reflecting on which of the lessons below have been the most useful to me, I offer my assessment of which 10 lessons were probably the most valuable to me over the past 40 years:
- Believing that I am worthy of care helps me take better care of myself and my T1D.
- More in: Attitudes & Beliefs
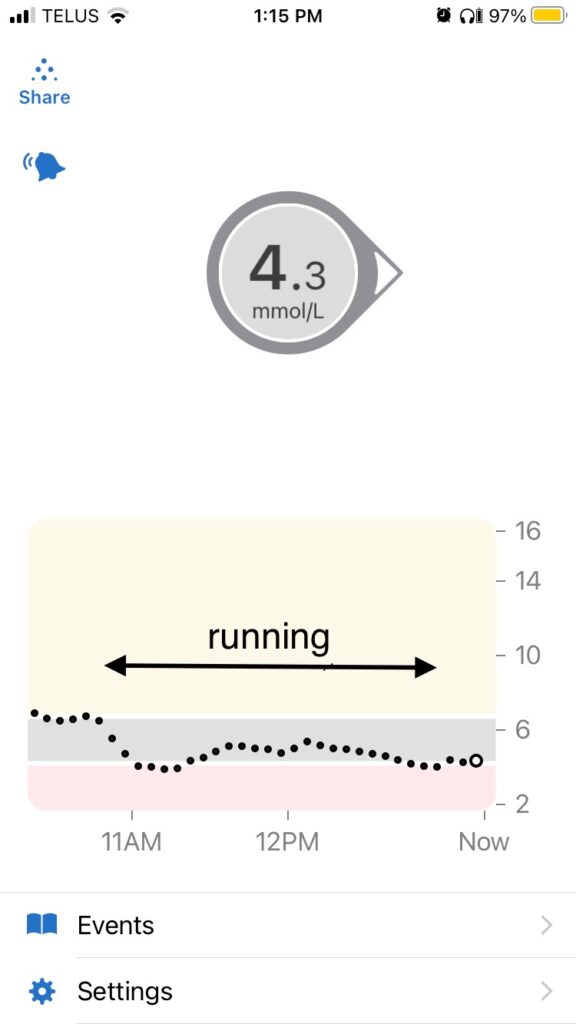
- I can exercise without going low even if I have insulin on board (IOB) by accounting for the fact that IOB gets multiplied by an average of 3X for me during exercise.
- “accounting for” = deliberately underdosing insulin to reduce the amount of IOB leading into activity and/or covering the multiplied IOB with fast-acting carbs
- More in: Physical Activity (Exercise) with Insulin on Board (IOB)
- The bolus strategy that works best for me when it comes to larger meals (>500 calories or so) is to bolus for carb grams as usual about 12 minutes before eating, then bolus for protein grams x 0.4 an hour afterwards, and fat grams x 0.9 three hours afterwards.
- More in: Protein & Fat
- Drinking 2-3L of water per day makes insulin, food, sensors, etc. work more smoothly for me.
- More in: Water
- T1D adds stress to my life and can be tough on my mental health. The best stress management and mental health support techniques for me are: exercise (I run a lot), sleep, getting outside, and connecting with others with T1D, either actively by communicating with others or passively by listening to podcasts or reading.
- More in: Mental Health & Stress Management
- T1D is going to consume more of my energy than I’d like. (What I’d like is for it to consume none.) I don’t have a choice about whether the energy consumption will happen, but I have some control over when it happens. When I put in energy up front by prebolusing, weighing food so my boluses are bang on, bolusing with post-meal activity in mind, and other such things, I can take it a bit easier afterwards, because T1D is less likely to suck energy out of me due to bouncing blood sugars.
- More in: Energy Up Front, Weighing Food, and Prebolusing
- Eating lots of fibre means I get to eat lots of good food, my meals absorb more smoothly with fewer spikes, and my insulin-to-carb ratio is substantially lower than when I don’t eat as much fibre.
- More in: Fibre
- Technology helps me tremendously. If I had to pick just one technology, it would be continuous glucose monitoring, but my closed loop (automated insulin delivery) system has been life-changing, and is one of the major advances made possible by combining pumps, CGM, and algorithms. My eternal gratitude to everyone involved in pushing this tech forward, especially the volunteers in the #WeAreNotWaiting community.
- More in: Technology & Tools and Looping
- When my settings are right, everything is easier. The easiest way for me to get my settings right is usually by starting from general guidelines (sometimes provided by my healthcare team, sometimes from literature), then taking notes on how things are working, adjusting as needed, taking more notes, rinsing & repeating.
- T1D is expensive, including in Canada. Staying organized about insurance and paperwork helps me minimize out-of-pocket costs.
- More in: Finances & Insurance
Attitudes & Beliefs
Shorter version: Taking care of my T1D requires taking care of myself. To do this well, I had to develop the belief that I am worthy of care. (next section)
Longer version: The most useful attitude for me for living with T1D challenges has been: I’ve handled other T1D challenges before. I can handle this, too. The most useful belief for me has been: I am worthy of care. I became much more able to manage T1D well when I started believing that as an adult.
In recent years, I’ve also done things to care for myself because I want to be here for my kids long-term. But for me, at least, the core belief that I had to acquire to truly take care of myself was that, regardless of who else is or isn’t counting on me, I am worthy of care for my own sake. (You are, too.)
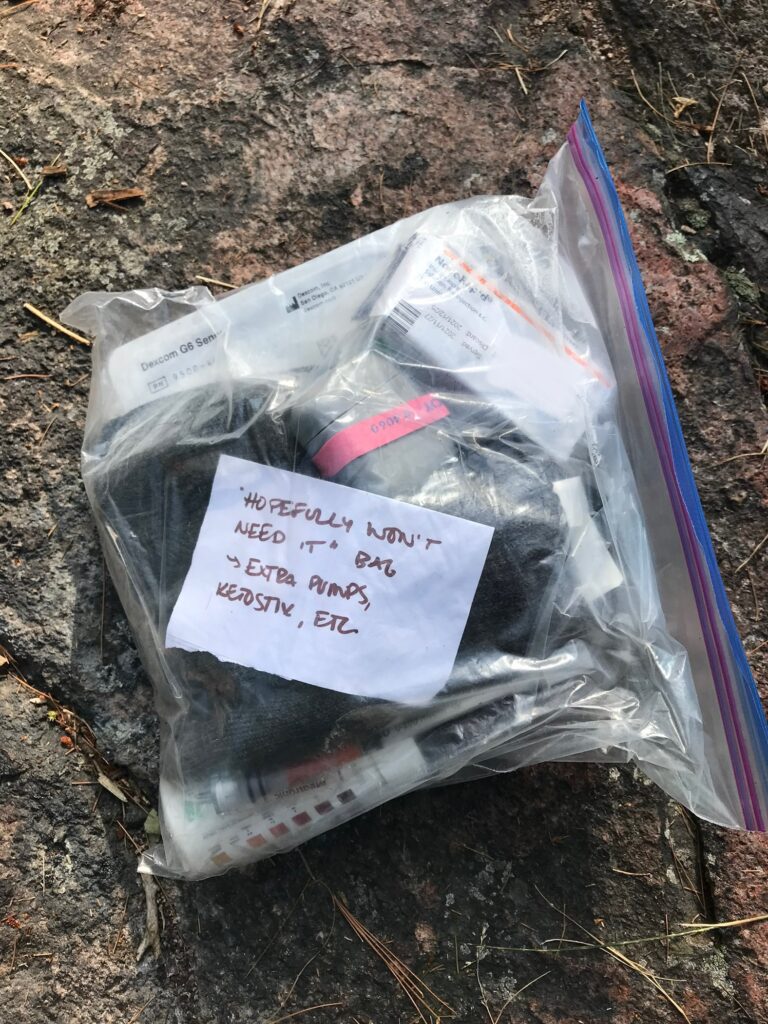
Backcountry Camping
Shorter version: For trips where water is plentiful, gatorade powder is light and efficient for hypo treatment/avoidance. Charging devices overnight can drain portable batteries unnecessarily, so it’s worth charging during the day. Morning oatmeal works ok with a longer (about 3x), smaller (about 50%) prebolus. Putting a silicon absorber in a dry bag with devices/supplies is cheap and can help protect from water damage in wet conditions. A 50% override (i.e., using only half of my usual insulin amounts, basal and bolus) seems to work well for both hiking and paddling days. I also increase my targets during backcountry trips for extra safety. You can’t turn off Share in the Dexcom app without internet so if the little red bubble is going to bother you like it bothers me, turn off Share before you leave cell range. I have found it comforting (when not needed) and useful (when needed) have plentiful backup supplies and screenshots of tech troubleshooting just in case. (next section)
Longer version: Backcountry camping is when you hike or paddle into the woods. You may end up days away from medical help. Frontcountry camping is when you can drive to your campsite or very close to it. Like most things, backcountry camping is possible with T1D, it just takes a bit of extra planning to do it safely.
I really enjoy being away from everything in the woods. It is the only time I am able to truly ignore thoughts of work I could be doing.
Over the years, I’ve typically managed to do one or two trips each year. I did a mix of kayaking, canoeing and hiking with friends or my dad as a young adult, a lot of canoeing when my kids were small, and now that my kids are older, we’ve done some paddling and some more ambitious hikes, and I’ve also gone out for a shorter time with friends.
My most helpful backcountry-related lessons have been:
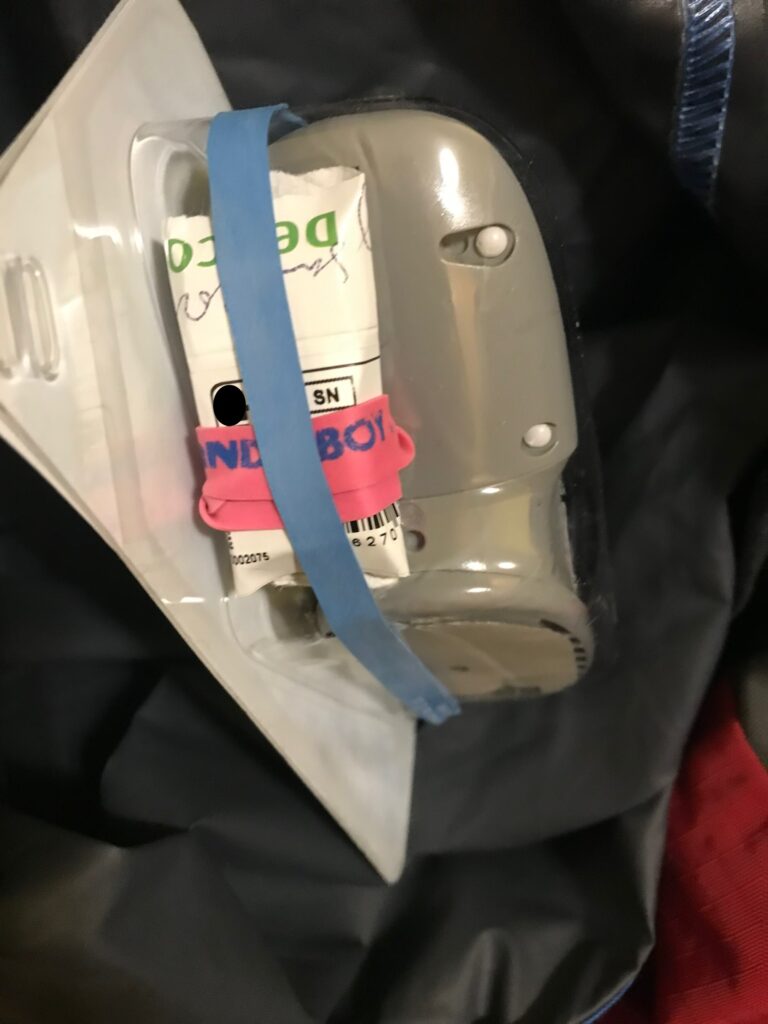
- Pack lots of backups. The downside is that I then have to carry them, but when I am days away from medical help, the peace of mind has been worth it to me and my family/group. With my current system, I bring one or more backups for each piece of equipment, plus backup long- and short-acting insulin so I could revert to multiple daily injections if needed. I show everyone on the trip how to administer glucagon if needed, and we agree on an easy-access place to always keep the glucagon. I bring at least two glucagon sources, plus gel that can be squeezed and rubbed into my cheek.
- Use Gatorade powder as my primary approach for treating/preventing lows. It’s lighter than most other low treatments. It would be bad news if the powder got wet, so I carry it in a small ziploc inside a larger ziploc, and the whole thing goes inside a dry bag of drinks and snacks. I mix it with treated or filtered water, then sip or drink as needed. On a 10-day trip this past summer, I used nearly a full can of powder by the end of the trip. (That level of use was as planned, and I still had other backup low treatments in the form of glucose gels, a few tubes of glucose tabs, some wrapped candies that fit nicely in a pocket while hiking with a heavy pack, etc.)
- Charge diabetes devices during the day, not at night. I learned this from a Backpacking Light podcast. Some devices (especially Apple devices, like my phone) will draw energy from a battery anytime they are plugged in, even if they are technically 100% charged. Plugging them in all night wastes power, which may increase the number of (heavy) rechargers needed.
- I can make oatmeal work without having to stress about leaving camp and getting moving right away (my former approach) by giving half my usual prebolus, doubling or tripling my prebolus time, eating the oatmeal, turning on a 50% override, packing up, then, if needed, drinking a bit of Gatorade before walking to balance out insulin on board.
- Diabetes devices go in dry bags with a silicon absorber. I use an older tubed pump, and I use this Aquapac case when canoeing. When hiking, I just bundle the pump and linkage device together into a small dry bag and have the tubing come out diagonally so I can fold over to maintain water resistance without compromising tubing.
- Some uncovered carbs are ok when working hard, but overdoing the uncovered snacks is a mistake. (Note to self: even though I am burning a lot of energy all day, gummi bears hit hard and require some insulin after 3 or 4 bears!)
- Overall, a 50% override is about right for me for most backcountry days. This means that I require about half as much insulin as usual when hiking/paddling all day; i.e., half the usual basal, half the usual bolus for food, and so on. Once at camp for the night, I typically turn it to more like 85%. I also increase my target from 5.0 mmol/L (90 mg/dl) to 6.3 mmol/L (113 mg/dl) and raise my suspend threshold from 4.0 mmol/L (72 mg/dl) to 5.0 mmol/L (90 mg/dl) for the whole trip.
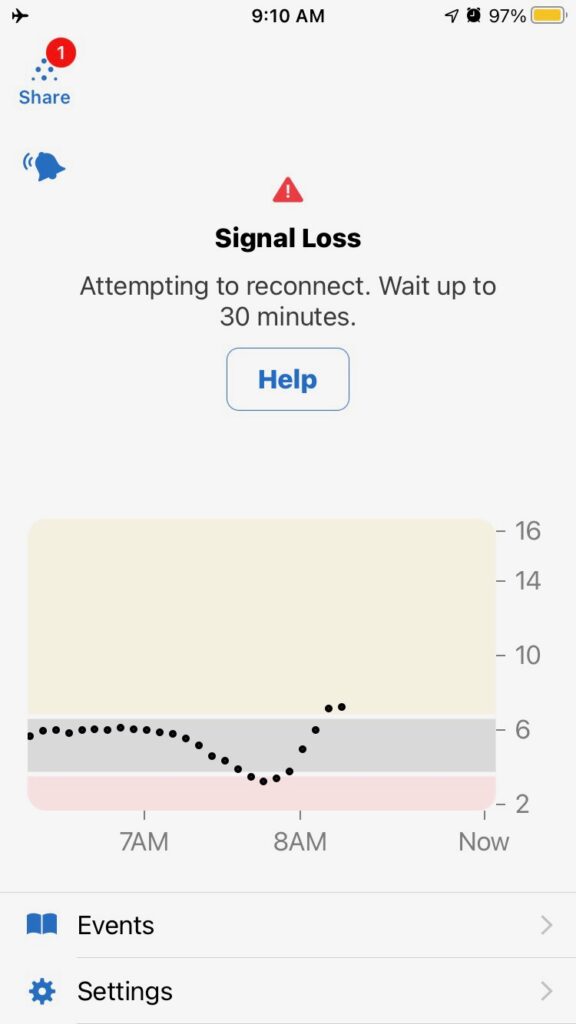
- Delete any previous transmitters and unused devices from my phone’s Bluetooth list to reduce the chance of signal loss and oh my goodness, turn off share BEFORE leaving cell range. You can’t turn it off without internet service, so when I forget to do it before leaving cell range, the Dexcom app spends the entire trip reminding me that my readings are not being shared. (Thanks, Dexcom, especially since the only person who follows my numbers is on the trip with me!)
- The dog carries his own food. (Uh, this isn’t really diabetes-related, except for the fact that I have to carry extra diabetes supplies, so it’s more important not to have to carry anything unnecessary. But since I don’t share photos of my kids, it’s an excuse to share at least a couple of cute photos.)
- Take screenshots of troubleshooting pages in Loopdocs before leaving so that I have that information in case I need it. This came in handy on a trip once when I had a lot of red loops.
- It saves time and phone battery to weigh things ahead of time and put the measurements in my food app in advance as custom foods labeled with the trip name (e.g., “[trip name] oatmeal day 1.”) I once tried writing the carb count on the individual meal bags, but too much of the writing rubbed off in the packed-full food bag, and I also couldn’t prebolus for breakfast when the record of the carb count was 10 metres up in the air. (Food is hung up overnight in the backcountry so that bears are less likely to be able to get at the food bag.)
Biggest Bang for the Buck
Shorter version: My top three T1D management techniques that give me the most benefit for the least effort required are: drinking lots of water, getting daily exercise, taking fast-acting insulin a specific amount of time ahead of eating. (next section)
Longer version: I sometimes joke to myself that I have three major priorities in my life (my family, my research & students, my health) and time for about two-and-a-half of them. My sad “joke” reflects the reality that I have to fit T1D and its many demands on my time alongside other things. So when I am going through especially busy, stressful times, I have learned that it is useful to focus on the things that give me the biggest bang for the buck when it comes to my health. By that, I mean that even though there are many things I might do with unlimited time, with constraints on my time and effort, I want to use my time and effort as efficiently as possible. Starting with the biggest bang for the buck, the things that I have found most helpful to me and my T1D are:
- Drinking plenty of water (time/effort: low, benefit: high)
- this is by far the thing with the greatest benefit for the least effort
- Getting physical activity every day (time/effort: high, benefit: very high)
- anything is better than nothing, but I only notice benefits to T1D if I get at least 30-60 minutes a day (hence high time/effort required)
- outdoors is best for mental health benefits
- Taking insulin at the right time (time/effort: moderate, benefit: high)
- multiple daily injections (MDI): taking long-acting at a consistent time each day (setting a reminder alarm if needed or attaching the habit to another time-based habit)
- pump & MDI: prebolusing 10-30 minutes for food (prebolus time may vary … for me, Fiasp takes 10-12 minutes, NovoRapid takes 30 minutes)
- Eating lots of fibre and protein (time/effort: moderate, benefit: high)
- fibre and protein really smooth out the way food absorbs, and they also help me avoid stress-eating too many carbs
- Sleeping decently (time/effort: high, benefit: very high)
- I need 8 hours but if I can’t get that much, some is better than none
- naps count as sleep
- when we had infants & toddlers (especially our first, who was not a good sleeper) my husband and I each had a predetermined 4- to 5-hour sleep window that the other person worked hard to protect
- Eating things that are somewhat predictable for me so that I can better match insulin to food (time/effort: moderate, benefit: moderate)
- figuring out a few reliable meals has really come in handy during times when I needed to simplify things
- here’s a list of things/recipes I like for anyone who would like to peruse for ideas
- Checking BG before and 1-2 hours after eating (time/effort: high, benefit: moderate)
- a CGM makes this easier, but I did it for many years with a meter
- Doing something for mental health (time/effort: high, benefit: moderate)
- physical activity and sleep can overlap with this, but sometimes I need to do other things for mental health
- Having routines & rituals (time/effort: very high to develop but low to maintain, benefit: moderate)
- I am a success-begets-success person, meaning I do better when I feel like I’m not a failure
- maintaining little routines & rituals makes me feel like a success at self-care, which makes it easier for me to tackle other, more time-consuming T1D tasks
This concept of focusing on the biggest bang for the buck also applies outside of T1D for me. For example, if I’m not feeling very energetic and I haven’t been sleeping enough and getting enough exercise, I focus on meeting basic recommendations for exercise (150 minutes/week; see also US guidelines) and sleep (7-9 hours a night) for at least a week or several before I start to consider other possible issues.
Burnout
Shorter version: I’ve gotten through burnout by riding it out as best as I could, and not beating myself up over it. (next section)
Longer version: When I’ve gone through periods of burnout, what helped me most was:
- accepting that my motivation was low at that time and not getting upset with myself about it,
- focusing on the basics: always taking insulin, testing at least twice a day (once I had a CGM, this became wearing the CGM), going for walks outside if possible,
- simplifying diabetes and life as much as I could in the current circumstances,
- getting extra sleep if I could, and
- repeating favourite meals and snacks over and over.
The repeated meals and snacks provided both comfort and predictability. I repeated meals and snacks that satisfied three criteria: 1) I like it, 2) I can afford it, and 3) I know how to bolus for it (or I can probably figure it out without too much effort.)
I am grateful that I haven’t had diabetes burnout in a long time, but I have definitely had times more recently when diabetes on top of everything else I was managing felt like a lot. Having some basics on which to fall back was really helpful in those times.
Comfort In, Dump Out
Shorter version: Sometimes, caregivers need a listening ear. In my view, ideally, they will seek that from someone other than the person with T1D. Based on my experience as a child, I would especially recommend that parents not complain to their children about how hard the child’s T1D is on the parent. Tell someone, but make it someone other than the child. (next section)
Longer version: One of the most helpful distillations I ever encountered about how to talk with people with health conditions was this article about what the authors called the Ring Theory. It is focused on traumatic acute health events, not chronic illness, so it doesn’t apply perfectly to my own experience of decades with T1D with their waxing and waning intensity. However, the central idea, “comfort in, dump out,” is a very succinct summary of how to deal with a wide variety of difficult health situations, including my experience of T1D. I know, for example, that my T1D occasionally adds stress to my husband’s life that he would not experience if I hadn’t brought my confused immune system to our relationship. While I acknowledge that my T1D has an impact on him, if he needs to vent to someone about that, it is better (for him and for me) when he seeks a discussion with someone who is not me; for example, a friend, his mom, another partner of an adult with T1D, or the like. The phrase, “comfort in, dump out,” has been a helpful way to succinctly convey this idea.
Complications
Shorter version: Human bodies are not made to last. T1D can wear our bodies out faster, and, as much as I hope my good adult BG control will help me, it can only do so much, especially given my childhood management. I find this to be an especially hard lesson to absorb, but there it is. (next section)
Longer version: If I go by definitions in scientific papers (for example, publications from the Joslin medalists’ study), I have no complications. My kidneys and heart are in great shape, I have no neuropathy (nerve damage), and no proliferative retinopathy. I feel really grateful for that, especially given the sub-par management during my childhood years. I also note that a lot of the science on complications of T1D suggests that while blood sugar management can help reduce risk of complications, the biggest predictor of complications is how long a person has had T1D. This is sort of like how age is the biggest predictor of things like cancer, heart disease, and other conditions. In other words, tighter blood glucose management may delay the onset of complications but if I live long enough, may not completely prevent them from ever happening. I’ve also seen science suggesting the variance attributable to glycemic indicators is lower than the variance attributable to genetic factors. In plain English, although I can (and do) do my best, the science that I have seen suggests that a good amount of whether I end up with complications comes down to how long I live, combined with the genetic lottery and the overall randomness of life. So I feel lucky thus far.
Although I don’t have any complications according to the above definitions, there are issues I have experienced or developed over time that I probably wouldn’t have or wouldn’t know about if I didn’t have T1D. The biggest issue that affects my life in a meaningful way is that I’ve had hypo unawareness for many years. I typically have no detectable hypo symptoms until I am truly, dangerously low. It usually isn’t until around 2.6-2.9 mmol/L or 47-52 mg/dl that I start to feel something. I have been told that this is likely linked to the repeated, severe hypos I had as a child. I deal with my hypo unawareness by using a continuous glucose monitor and being really careful, especially if I need to drive or travel solo. (Also see the section titled Hypos.)
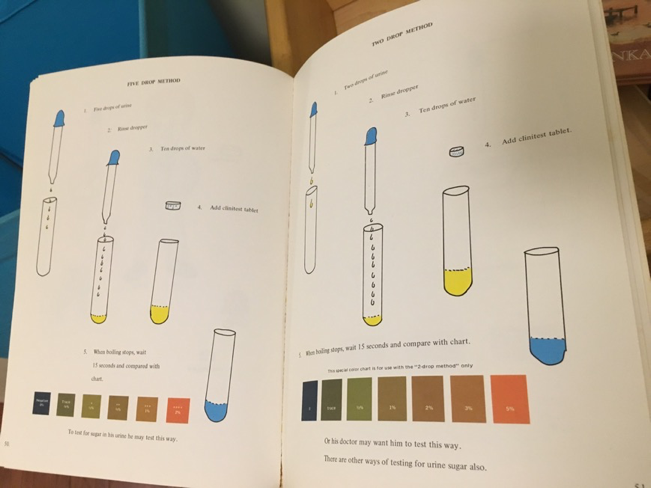
I also just got my first diagnosis of mild nonproliferative retinopathy (formerly known as, “background retinopathy”) recently, which threw me, even though it probably shouldn’t have. I know that this is extremely common, especially for those of us long-term T1Ds diagnosed in the era of urine testing and NPH insulin. It is so common and such a non-issue that, in studies of people with long-term T1D, the analyses often lump all the least-affected people into one category, combining mild nonproliferative retinopathy and no retinopathy together. The Wisconsin Epidemiologic Study of Diabetic Retinopathy (which studied people diagnosed before or around the same time as I was) reported that 97% of people with T1D had at least a little bit of retinopathy after 25 years, so I feel fortunate to have made it to 40 years. (I still preferred the comments, “Are you sure you’re diabetic? I can’t tell from your eyes!” I got for 39 years.) I’ve since had follow-up testing to confirm that it’s extremely peripheral, so that’s good news, because as long as it isn’t progressing, it is very unlikely to ever be a problem, and may well never need treatment. The retina specialists also noted that they’re only able to detect it thanks to advanced testing methods. (“If we were using the technology we had 10 years ago, we wouldn’t have found this.”) Hopefully I will be like most people diagnosed at this point: it will remain stable, I won’t need any treatment, and it won’t progress beyond a little bit at the edges. If I’m in the minority of people who do need treatment at some point, the treatments available these days are very good, and have greatly reduced the number of people who will experience vision loss compared to previous generations of people with T1D. My husband also pointed out, “We’re not built to last forever,” which I found oddly comforting.
And yet, this news still gave me the chance to learn some more about living with T1D. All my life, I’ve heard statements about, “the complications that will happen if you don’t take care of yourself.” I’ve never loved that expression, because it propagates the myth that diabetes complications are meritocratic—that the only people who end up with complications “deserve” them. (This is similar to how people with type 2 diabetes are often blamed for their condition, with little to no acknowledgement that we are not all dealt with the same genetic hand and, thanks to different conditions of life, we are not even all playing the same game.) On top of that preexisting dislike, it meant that when one of the scary complications finally made a little crack in the thick barrier I’d carefully constructed and defended over decades, I felt betrayed. I’ve taken excellent care of myself for many, many years. It was especially hard emotionally because my childhood management was not great, and if there’s a causal relationship at play here (rather than just the random nature of biology or genetic luck) the medical neglect I experienced during childhood is most likely what kicked off a slow progression that brought me to now. So I feel sad about the support I needed but didn’t get as a child. It’s also possible that my hypo unawareness (also linked to my childhood management with its repeated severe lows) may have contributed to this diagnosis, as low blood sugar can contribute to eye damage among people with diabetes.
In any case, the main thing I learned from this news is that it is useful to allow myself to feel the feelings I have, to reach out for help when I need it (many thanks to the colleagues who helped me put the news in perspective) and to avoid getting too cocky about excellent blood glucose numbers. There are still no guarantees.
Consistency
Shorter version: Consistency beats perfectionism every time. The only things that have ever helped me in T1D management are the things I can do consistently. Burning myself out in fruitless attempts at perfection has never been useful. Being consistent requires being realistic with myself. (next section)
Longer version: I don’t know if there is research on this, but anecdotally, it seems that perfectionism is common among people managing T1D. I wonder if part of it comes from being repeatedly invited to reflect on your mistakes. I have definitely had the classic experience in which a health professional points to a BG from last month, and asks me, “What happened here?” I suspect that for those of us with a preexisting tendency towards perfectionism (also known as: a fear of never being good enough), those well-meant interactions may have created unhelpful thought patterns.
Whatever the cause, I have definitely learned over the years that T1D perfectionism is not helpful to me. Consistency, on the other hand, is extremely helpful. Consistency requires me being realistic with myself about what I can do on a regular basis. It also means I have to face the fact that I am overly fond of novelty. I deal with my desire for novelty by (a) running small experiments that make the same-old-same-old feel at least vaguely new and (b) being middle-aged and recognizing that this is part of life.
Control
Shorter version: BG control is possible. It does not guarantee control over all outcomes, but it does make life easier in the short term. (next section)
Longer version: Probably the hardest lesson of T1D (and one that I seem to have to re-learn every so often, see my note above about retinopathy) is that I can do everything “right” but that does not guarantee I will get the results I want. I only control my efforts. I don’t control the outcome.
That said, I’ve definitely learned over the years that blood sugar management is possible. If my current approach isn’t working, I change my approach. I am always confident that a solution exists, even if I haven’t found it yet. I’m not always very happy about it, but I’ve learned over the years that sometimes, the only way out is through.
Working towards BG control is worth it to me because having reasonably level BGs feels much, much better to me than bouncing around. Bouncing around really drains my energy. The energy boost of staying level is extremely noticeable. When I got my first pump and could fine-tune my basal insulin to suit my body’s needs, I once said, “If this is what nondiabetic people feel like all the time, they should be doing more with their lives!”
Daily Kit
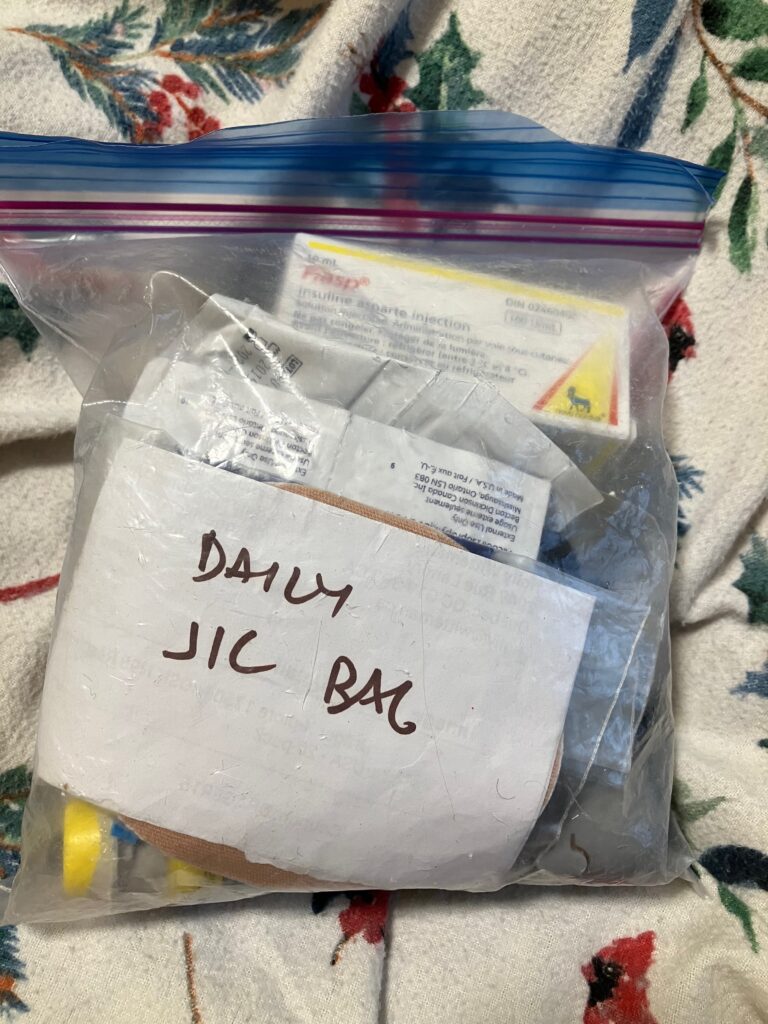
Shorter version: It cuts down on my packing time and decisions to have a small pre-packed kit that lives in my backpack. I also have a small number of bare minimum essentials I take with me everywhere, tucked in a pocket or purse. (next section)
Longer version: I have always found it useful to keep a daily “just in case” kit in a small ziploc that goes everywhere with me. Back in the day, if I was going out for the night, the absolute bare minimum supplies would go in my pockets or purse (glucose tabs, test meter, some strips, a lancet, pen or a vial of insulin and syringe.)
My current usual daily kit has a spare pump battery, a syringe or two, my current vial of insulin (unless I’m going out in very cold weather) with cartridge pieces in the box, a spare linking device to connect my pump to my phone, inhaled glucagon, one or two infusion sets, a sticker to go over my dexcom, some alcohol swabs, a nickel (for removing pump caps), and a bit of cash (just in case.)
Data & Reports
Shorter version: Reviewing my continuous glucose monitor patterns once every week or two is a really helpful habit for my T1D management. It is very easy now that I can check the Clarity app on my phone. I almost never looked before, but now it’s an easy weekly habit. (Thanks for making it available on my phone, Dexcom engineers.) I look at my average BG, standard deviation, Ambulatory Glucose Profile (AGP), and sometimes my Overlay and Compare report. (next section)
Longer version: I am so happy that Dexcom put their Clarity reports into a smartphone app. Prior to that, I knew that looking at my data regularly was a good idea, but outside of pregnancy, I had never been able to prioritize it as a regular habit. Now that I can quickly pull it up on my phone, I have found that glancing at my data at least once every week or two helps me quickly identify anything that might need tweaking. I usually look at the Ambulatory Glucose Profile (AGP) for the past 14 days, and sometimes the past 7 days if I’ve had a recent change and want to see how it’s going. I also like the Overlay report, because I can look at each day, and the Compare report, because it’s helpful to see if a change I made is having the desired effect or not. I have learned a few useful tricks about using the Clarity reports from the free webinars that Dexcom Canada put out with some experts I know and trust.
I wish they hadn’t dropped standard deviation from the AGP, but at least you can still see it in the Clarity app’s Summary page. I think standard deviation is an underused summary statistic, possibly because too many people don’t understand what it means. Standard deviation is an index of dispersion. In plain language, if you’re looking at your BGs over two weeks, standard deviation shows how far your BGs are from your average across those two weeks. A bigger standard deviation means you have more BGs far away from your average. A smaller standard deviation means your BGs are clustered closer to the average. I’m always happy when my standard deviation is 1.7 mmol/L or lower (31 mg/dl or lower.) The one thing I am careful about when looking at my standard deviation is that, for example, if I have a day running high and then a day running low, the 2-day standard deviation will be similar to what I’d see if I’d spent two days bouncing from high to low, but the solutions to those two situations are likely very different. Summary statistics only tell part of the story. I always look at the graphs as well as the summary statistics. (This also applies to data in my job. I sometimes show students Anscombe’s quartet when they have failed to plot their data before running summary stats. The Datasaurus dozen is also a very funny illustration of this issue.)
Back before I had a CGM, the one time I looked at my data regularly was during pregnancy. I used to pull out my finger prick BG data from the database and built a script that organized it into a spreadsheet by hour of the day. It helped me see patterns that I might not have noticed otherwise. I suspect that many meters now do that on their own with no need to write a script. Knowing what I know now, if I wanted to review the data I had available without a CGM, I would again find a way to review multiple days on a timeline to look for patterns, and I would also keep and review notes a little more aggressively than I do now.
I still have not gotten around to setting up Nightscout again, but I keep meaning to do that. If I were starting from scratch these days, I would use either Nightscout or Tidepool.
Energy Up Front
Shorter version: I find it easier to put in effort (energy) ahead of time to avoid having T1D suck energy from me. (next section)
Longer version: T1D is going to take some of my energy. There’s no getting around that. It just is. The reality of the condition is that it takes energy. My choice is: do I deliberately spend the energy up front to manage my BGs, or do I let my BGs bounce around, sucking energy out of me? I do not love my options here. I would rather not have this condition withdrawing energy from me. But since it’s here and I can’t do anything about its presence, I choose to put in energy up front. This includes doing things like weighing food so that I can set it & forget it with my boluses, planning exercise into my day, choosing mostly food that works well and/or has a predictable impact on my BGs, and so on. I wish I could just live a spontaneous life and not have to spend energy on T1D, but that is not an option on the table for me. T1D is going to take energy, no matter what. The only choice I have is whether I put the energy in up front, or the energy gets sucked out of me later. So I choose to put energy up front.
Fibre
Shorter version: Fibre is really good for everyone, and has extra benefits for those of us with T1D. Eating ~40g/day helps me keep my BGs level. When I had to eat low fibre for a week recently, my daily fibre intake dropped by 74% and my insulin-to-carb ratio increased by almost exactly the same percentage (70%), even after accounting for subtracted fibre grams. I get the best results when I subtract 50-100% of the fibre grams from the carb count, depending on what kind of fibre it is. (next section)
Longer version: Fibre is really good for most people, not just those of us with T1D. It is specifically recommended to help prevent heart problems (extra important with T1D), many cancers, especially colorectal cancer, and, relevant to those of us with any type of diabetes, blood glucose management. As I understand it, it is not only that fibre itself doesn’t get digested, it also prevents the BG effects of a portion of the non-fibrous carbs and fat. I think of this as fibre sort of soaking up some of the carbs and fats.
I had the chance to personally observe the benefits of fibre for blood glucose management recently when I had to follow a low-fibre diet for a week to prepare for my first colonoscopy. I typically eat very high fibre. My average is 40g/day, which is smack in the middle of the recommended amount for people with diabetes (link in French) where I live. When my daily fibre intake dropped by 74% for a week, the insulin my body needed per gram of carbs increased by 70%. This included foods like a particular kind of yogurt (with zero fibre) that I eat all the time, so it was extremely clear exactly how much my insulin-to-carb ratio had changed. I had not fully realized how much I was reducing my insulin needs just by routinely eating high-fibre foods.
When I’m not preparing for cancer screening, my family and I eat a lot of beans, lentils, fruit, vegetables, and whole grains. As I understand it, the reason fibre helps with blood glucose management is twofold. Many people with diabetes are taught that not all of the fibre will convert to glucose, so you need to subtract fibre grams when counting carbs. But in addition to that, fibre slows (and may prevent) some of the whole meal’s conversion to glucose, meaning the whole meal takes longer to digest and may not hit as hard overall. For example, I made black bean brownies recently using 4 cups of cooked black beans across 16 brownies. Sixteen brownies made for four meals’ worth of desserts for my family of four. Observing the effects across four meals, I found that having them for dessert with some berries reduced the impact of the whole meal on my BGs by about a third to a half.
In general, for any meal with a decent amount of fibre (which is most meals for me), I know to expect gentler, slower digestion, and also to subtract 50% to 100% of the fibre grams from the carb grams. I first learned to always subtract 100% but I have learned over time that this is too simplistic. The percentage depends on whether the fibre is mostly coming from insoluble fibre (e.g., whole wheat bread, brown rice), in which case I may subtract up to 100% of the fibre grams, or whether it’s coming from soluble fibre (e.g., chia seeds, oatmeal, lentils) or mixed foods (e.g., most beans, nuts, fruits), in which case I subtract 50-75% of the fibre grams. This is not an exact science, and if I have a mix of fibres, I just guess partway between fully and partially subtracting them. These are not incredibly large differences, so I don’t worry too much about getting it perfect. For example, if I’m eating a meal of 60g carbs with 8g fibre, bolusing for 52g, 54g, or 56g carbs is not wildly different.

Finances & Insurance
Shorter version: T1D is expensive, including in Canada. It is in the interests of insurance companies to make us give up. I have learned I can minimize my out-of-pocket costs by keeping a spreadsheet, a file of notes (with dates of calls and whom I spoke to), and being persistent. (next section)
Longer version: Health care in Canada is sort of public. Things that happen in hospitals, doctor’s offices, and other publicly-funded health care spaces are typically funded by taxes. Things that happen at home (i.e., almost all of T1D management) are only sometimes funded by the public system. What is funded or not funded varies by province. (The way I typically explain Canadian health care to people in the US: each province/territory is basically a big HMO for its residents. If you’re interested in more details, here’s a paper I co-authored that describes the system briefly under the subheading “Canada’s healthcare system.”) Most people have “extended health benefits” (insurance) through work or school to cover things like medications and devices. Throughout my life, I have been in a variety of different situations, from having lots of extended health benefits to none. The most useful things I have learned over the years with respect to finances and insurance are as follows.
I find it useful to keep a spreadsheet of insurance claims. My spreadsheet has service date, date submitted, what it was for, date of the photo or document scan (so I can find it in my files if need be) and then several columns for how much I got back, and follow-up actions taken (e.g., calling the insurance company, submitting the uncovered amount to my husband’s insurance, etc.)
Insurance companies count on you giving up. If you give up, they win. If you don’t give up, you may win. When I was a graduate student, the insurance company that covered graduate students told me our plan would cover 80% of an insulin pump, so I went ahead and got one, only to have them then say I had misunderstood and they weren’t going to cover any of the $6000 cost. I spent hours and hours and hours on the phone over months. It was so frustrating and exhausting. I finally got them to pull the recording of the call in which I was told it was covered. They paid $4000. I did not enjoy being out 2k, as that was almost 10% of my annual grad student stipend, but it was better than being out 6k.
I have found it useful to keep a running document of all phone calls and emails. I record the date and time, the name/employee number of the person with whom I am speaking, and a summary of what was discussed. I can pull up that file as needed and refer to previous conversations. I find that after a couple of years with a given insurance company, most of the wrinkles get ironed out, but this document is invaluable in the first few years. My work has changed insurers three times in the last decade. Every time, I had to start over with this smoothing process.
There have been times in my life in which there were programs that could have helped me (e.g., when I had no extended health benefits) but I didn’t know about them and didn’t know to ask. I wish I had asked. Health professionals can often help, other people with T1D are often very knowledgeable, and some of the most knowledgeable people about these programs are device representatives, so trying to get get an insulin pump is a great way to find out about different funding programs.
I oriented my career around always having extended health benefits, and being able to budget to pay out of pocket for things that insurance does not cover or does not cover fully. For example, I paid a lot out of pocket for continuous glucose monitor for a long time. I find it frustrating that the various provincial systems have these enormous gaps in coverage, so I do what I can to promote better coverage while also recognizing that nothing is going to change in the short term, so it’s in my and my family’s interests to do what I can to put myself in a position to have insurance coverage. I love my job and I do not regret my choices, but I might be doing something very different if I weren’t extremely aware that I have an expensive chronic condition.
Life insurance is often very difficult for people with T1D to get. I can’t even get supplemental group coverage through my work. Any type of diabetes automatically disqualifies me for coverage beyond 3 years’ salary. In Canada, there is exactly one company that will insure people with T1D: Canada Life. My husband and I have paid for private coverage from them since I was pregnant with our first child. It is a substantial part of our budget, and I somewhat resent that, but I am also grateful that there is at least one insurer.
Highs & Spikes
Shorter version: My favourite way to bring down a high is to take a 50-80% correction and then do something involving large muscles like walking, bicycling, or squats. The insulin will be in there for hours, but the effects of the movement stop as soon as I stop moving, so I can bring my BG down quickly and stick the landing. Similarly, if I’m not able to prevent a spike by bolus timing, I can typically just add a walk after eating. (next section)
Longer version: I am grateful that I rarely have stubborn highs these days. (Thank you, Loop.) But I’ve had them at times, and the best approach I found for bringing them down has been: if there are ketones, I follow a ketone protocol. If I don’t have ketones, I take a correction, drink 500mL to a litre (2 to 4 cups) of water, go for a walk, ride my bike slowly, or, if I’m really crunched for space or time, do squats. Any movement speeds up insulin action, but using large leg muscles is especially good.
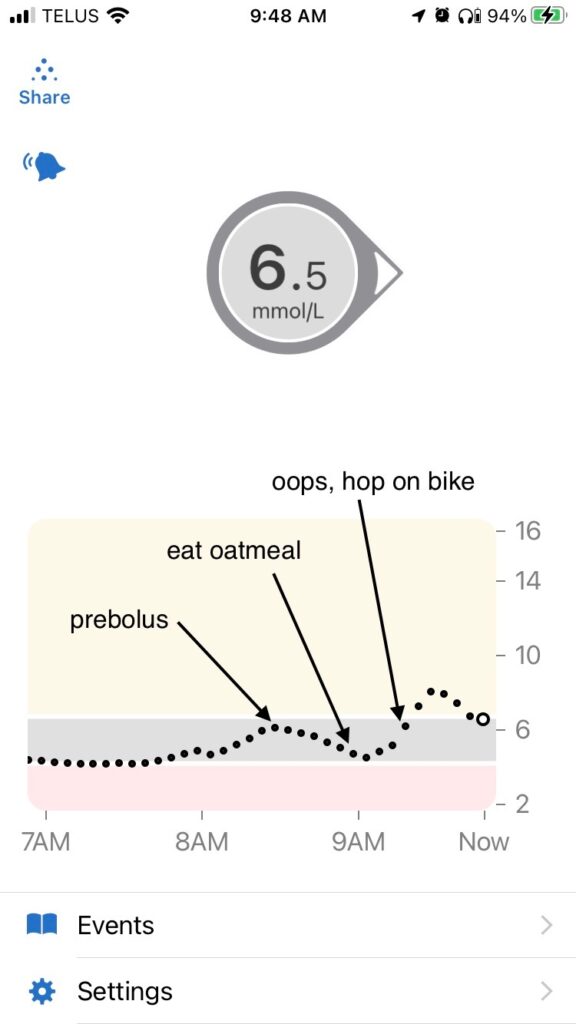
I use a similar approach for blunting spikes. For example, if I am not able to prebolus for some reason, or if I make a mistake in how I plan a bolus, I can often correct it afterwards by adding a bit of activity. Below is a recent example of what that looks like. I was experimenting with timing high-carb breakfast (oatmeal) on days I don’t run in the morning, and I got the timing wrong, so I fixed it afterwards with a bit of leg movement to boost the insulin, also known as riding-a-stationary-bike-while-answering-emails. Before I had the bike option, I would have used walking or squats instead. I can also answer emails on my phone while doing squats. #BizarreAcademicSkills
For folks in countries that use mg/dl:
10 mmol/L = 180 mg/dl
6.5 mmol/L = 117 mg/dl
6 mmol/L = 108 mg/dl
4.2 mmol/L (bottom of my range) = 76 mg/dl
What I especially like about using a combination of insulin and activity to deal with highs and spikes is that, unlike insulin, activity starts working immediately as muscles suck up glucose, and its effects stop very quickly when I stop moving. There is some residual increased insulin sensitivity after a lot of activity, but I’ve never had light walking, biking, or squats do anything to my sensitivity after I stopped moving. In other words, while I can sometimes overshoot (pun intended) when using insulin alone to treat a high or spike, I can be more precise when using less insulin combined with some activity. This allows me to bring down higher BGs faster without going low.
Hypos
Shorter version: My best way to avoid hypos is to avoid needing great big correction boluses. Looping is a huge help. The fastest hypo treatment for me is sweetened chalk glucose tabs. (next section)
Longer version: I’m completely hypo unaware and have been for almost two decades. I’m told that this is likely linked to my frequent severe hypos as a child. One of my main repeated childhood memories is coming to consciousness, vomiting from the glucagon, and then spending the rest of the day throwing up. Fortunately, I haven’t needed glucagon as an adult, but in the years before I got a continuous glucose monitor, I did have two severe hypos, one while 14 weeks pregnant with my first child and one while traveling solo. A few years ago, I also started having really unpleasant post-hypo hangovers in which I am intensely, unshakeably sad for several hours after a hypo. So I am really motivated to avoid hypos in the first place and to treat them as quickly as possible when they happen.
I find that the best way to avoid hypos is to avoid highs. It sounds bizarre, but by doing things to avoid going high or treating a rise as quickly and early as possible, I don’t accidentally overtreat the high because my absorption was different, my sensitivity was a little off, or something else went pear-shaped. Loop (see section: Looping) has helped enormously with this. It basically automated and refined what I was already doing.
For treating hypos when they do occur, here are my personal observations from many years of experimentation:
- Best for quick recovery: glucose tabs + a drink of water
- Note: Water helps any hypo treatment hit me faster. I was given this tip many years ago by a certified diabetes educator who herself had T1D. If the treatment is a gel of some kind (glucose gel, honey), I find it also helps to put into the pocket of my cheek and rub my cheek from the outside.
- Least likely to overtreat with: glucose tabs, because, unlike my kids when they were toddlers, I will never eat these unless I have to
- I let both my kids try my glucose tabs as toddlers (I made this mistake not just once, but twice!) mistakenly thinking that, once they tasted them, they wouldn’t ask for them anymore.
- There was a time in my life when I just could not choke down glucose tabs anymore and moved to lifesavers for a number of years. Lifesavers were better than nothing but they were not as fast as glucose tabs and I was more likely to overtreat. These days, I am back to glucose tabs as my first choice.
- Best for running: glucose gels
- Most likely to make a gooey mess in my pocket after I forget they are there: glucose gels
- Best for someone else to give me in the night: juice box with a bendy straw
- Best add-on to help avoid repeat lows: peanut butter on: toast, apple slices, or a spoon
- Most enjoyable while treating: cereal and milk
- Most likely to overtreat and regret it later: uh, cereal and milk
Insulin
Shorter version: I have found it helpful to try different insulins, pay attention to how different insulins work in my body (when they peak, how long they last), track how different injection/infusion sites perform, rotate my sites by switching sides each month or each sensor change, and be aware of rules of thumb in the book Think Like A Pancreas by Gary Scheiner. (Click here to jump to a summary of the rules of thumb.) (next section)
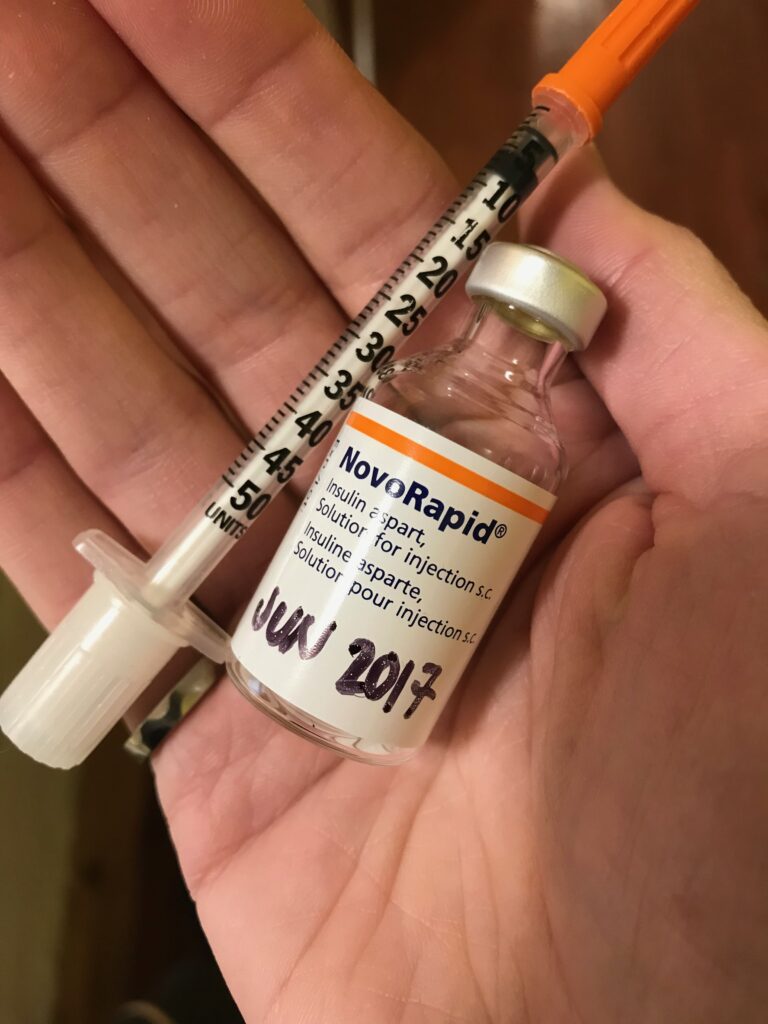
Longer version: I have always found it useful to try new insulins when they come out. I am not usually lining up to be the first person in Canada to get the latest vial, but I do like to give new options a try at some point and see if they are better than what I had used before. I started on the old beef & pork insulins (Toronto and NPH), moved to human synthetic insulins (R and N), used different long-acting insulins (Lente, Ultralente), used Humalog in pens, and since I started pumping, I have used Humalog, NovoRapid (also known as Novolog elsewhere), and Fiasp. I am currently using Fiasp. It find it stings a little occasionally, but the speed is worth it. I like that it starts a bit faster. I do not like that my sites don’t last as long. I also do not like that it still lasts 5-6 hours. I am contemplating giving Apidra a trial, as I’ve seen some data suggesting that it can clear faster.
I have found every insulin to be at least slightly different. I need a bit more or less of different insulins, they differ slightly in how long they take to start working and how long they take to clear out of my system. This also varies by how much I take. I find that bigger boluses often seem a bit sluggish to get going for me and then, once they start, they hit hard. But by and large, all the insulins I’ve used in the past couple of decades (Humalog, NovoRapid/Novolog, Fiasp) take about 5-6 hours to clear my system completely. Setting duration of action to be shorter is a recipe for me to have trouble with exercise and insulin on board. So the most useful thing I have learned is: when trying a new insulin, pay close attention to when an insulin peaks, and when it is done working.
I find that insulin action also varies by where I inject/infuse it:
- my most predictable (i.e., least variation from one bolus to the next) locations: on my hips and around towards my back
- my fastest infusion site location: belly (I will also occasionally use my upper abs, but it’s harder to find a comfortable spot there)
- my fastest injection location: legs (this would probably also be my fastest infusion site but I cannot deal with sets on my legs … it’s way too close to muscle for comfort)
I use this knowledge as needed. For example, as noted above, I don’t put infusion sites on my legs because it just isn’t comfortable for me, but last year when I had a site failure and spiked up to 15 mmol/L (270 mg/dl), I grabbed a needle, injected 2 units right next to my quad, and hopped on the stationary bike I use for zoom meetings. My BG was back down within half an hour and I didn’t go low.
To rotate infusion or injection sites, an insulin pump trainer who herself had T1D gave me the tip: pick one side of my body for one month, then the other side of my body the following month. I did that for years. Once I started putting my continuous glucose monitor on my arm, I switched to putting my site on the same side as the CGM instead.
All my amounts and ratios are fairly textbook on the lower end of what’s expected in the standard published formulas. I really, really like the book Think Like A Pancreas by Gary Scheiner, which explains the textbook calculations in detail. (My only problem with the book is its insistence on testing everything on days with no activity, no menstrual cycle, no stressful or exciting events … I end up with no options available!) When I first read it long ago, it helped me understand recommendations from my diabetes care team and helped me speak their language when I explained adjustments I’d made. The key formulas I have found useful are the following. (Note that these use weight in kg. If you use lbs, you can calculate your weight in kg by taking your weight in lbs and dividing by 2.205. This means the number representing your weight in kg is a lot smaller than the number representing your weight in lbs. For example, 150 lbs is about 68 kg.)
Formulae in Think Like A Pancreas, and what I have learned about their accuracy for me:
- Total Daily Dose (TDD) for very active adults is listed as typically 0.4-0.8 units of insulin per kg of body weight. For moderately active adults, it is 0.5-1U/kg. For inactive adults, it is 0.6-1.2U/kg.
- This is accurate for me. I am very active and my TDD runs around 25U on average these days, or about 0.4U/kg.
- That average is very much an average. My actual TDD varies depending on things like activity, hormones, and food. Most days it’s somewhere in the range 23-27U, but in the past year, I’ve had TDDs under 10U (hiking trip days) and almost at 40U (sedentary travel days.) I find it helpful to glance at my TDD routinely so that I have a sense of my normal variation. This helps me see patterns that are unexpected due to hormones or illness.
- Total daily basal insulin for very active adults is listed as typically 0.15-0.4U/kg. For moderately active adults, it is 0.2-0.5U/kg. For inactive adults, it is 0.2-0.6U/kg.
- This is accurate for me. My total daily programmed basal insulin is 0.18U/kg. (My actual basal varies because of how Loop works, but I have tested those basals recently and know they are right.)
- Estimated insulin-to-carb ratio (I:C ratio) is 1 unit to 850 grams of carbs per kg of body weight.
- That’s almost exactly accurate for me in the morning. My I:C ratio is 1:865/kg in the morning. It’s too much insulin for me with my usual way of eating the rest of the day. My I:C ratio is 1:1200/kg the rest of the day.
- However, when I had to eat low fibre for a week, the Think Like A Pancreas estimate was not enough insulin, so I suspect my overall ideal I:C ratio for a more typical diet (given that most people get less fibre than the recommendations but a bit more than a low residue diet) would probably be pretty close to 1:850/kg.
- Estimated insulin sensitivity factor (ISF), meaning how far one will fall after taking 1 unit of insulin, is 94/TDD in mmol/L (1700/TDD for mg/dl), and it’s typically 30%-50% higher (meaning most people need 30-50% less insulin) at night
- This is a bit too much for me, though the 50% less insulin at night is correct. My ISF is 111/TDD most of the day, 100/TDD in the morning, and 143-154/TDD overnight.
When I am testing and adjusting, I keep notes. I am not always great at making the space in my head to remember all these details. Also, given how long I’ve had T1D, it all starts to blur together. So I deal with this by keeping notes. I have done it in a little book, but these days, I use screenshots of settings screens in which I add little notes using the edit image function.
Logging Food
Shorter version: For years, I thought logging food sounded like a pain. But then I was inspired by someone who had lived well with T1D for 70 years, so I gave it a try. It was a bit of work to get started but now it’s just part of how I manage, and it’s really helpful to me at my current stage of life and T1D. (next section)
Longer version: I only started logging food routinely in the past decade. Previously, I had always disliked being asked to bring in a food record to a dietitian consult. I once instead brought in 2 weeks of photos of my vegetable-filled plates. They didn’t ask me for a food log again.
I think because I associated it with being annoyed, I thought of logging food as a pain. However, once I decided to make an effort and got in the groove of it, it has become a quick & easy habit and really helpful for my T1D management.
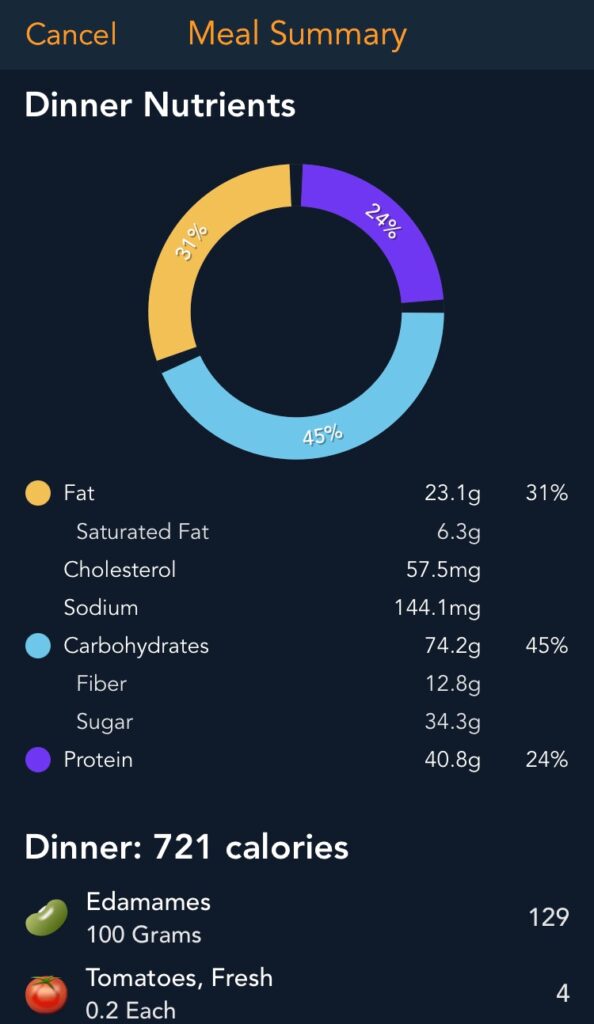
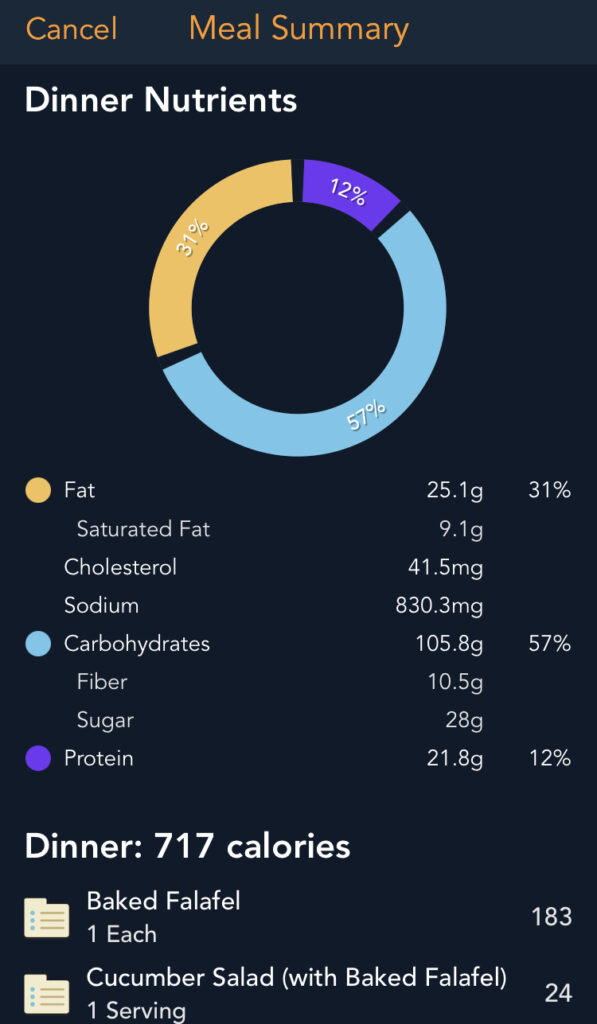
I was inspired by an older gentleman who, when I met him, was 71 years old, had lived for 70 years with T1D, and was in great shape. We were at a multiday meeting together, and I noticed at mealtimes how he jotted down everything he ate in a little notebook. I really liked his attitude and how well he was doing, so I decided to give it a try, and started using a food logging app. I was initially motivated to do it to get more precise carb counts, but I’ve ended up using it for all sorts of purposes—refining fat and protein boluses, figuring out exactly how to modify I:C for fibre, making sure I am getting enough protein, and losing weight when I decided to do that. (See section: Weight Management.)
Logging food can promote disordered eating or disordered thinking about food, so I’m not sure it’s right for everyone. There were times in my life when it would not have been right for me. But it is very helpful to me at my current stage of life. I’m glad I decided to finally start doing it routinely.
The app I use is called Lose It. It was the first one that came up when I searched for a food logging app, all of which seem to be oriented around weight loss. This one looked like it would make it relatively easy to put in my own recipes and repeat combinations of foods so I don’t have to enter everything by hand every time. It’s reasonably easy to use and I really like the ability to call up combinations of foods and recipes I’ve made before. I don’t love all of its features, but it is fine. I don’t know if it’s the best such app, but I’m now committed by the fact I’ve spent years entering recipes and would not want to start over in a new app. (It has an API and I occasionally wonder how much work it would be to port the data directly into my automated insulin delivery system…)
Looping
Shorter version: I use Loop, one of the do-it-yourself automated insulin delivery systems. It has been life-changing. For anyone who can access the tools, I highly recommend trying a do-it-yourself or commercial automated insulin delivery system. Available commercial systems vary by country. Here’s a good write-up with links to the various do-it-yourself systems out there if you are interested. (next section)
Longer version: I started looping (using Loop, one of the three main do-it-yourself automated insulin delivery systems out there) four years ago. Every 5 minutes, the system analyses the estimated blood glucose from my continuous glucose monitor, makes a prediction about where my BG will go based on what I have told it about food and settings and what it can see in my current trajectory, and adjusts accordingly, adding a bit of insulin if I might need a bit more, reducing basal if it thinks I might need a bit less. I can also crank my insulin up or down by a set percentage if I want to. It has been life-changing. I offer my undying gratitude to everyone who has helped to bring these systems to the community. I had very good control before Loop, but Loop has brought me some fantastic benefits:
- fewer lows
- easier time exercising
- uninterrupted sleep nearly every night
- I cannot emphasize enough how amazingly life-changing it has been to be able to sleep through the night almost all the time.
- the ability to set overrides (% increases or decreases of overall insulin) and/or to bolus from my watch
- This is incredibly useful in meetings at work when it is tricky to pull out a phone, when doing things outdoors in cold or wet conditions, or while out bicycling, running, commuting, walking, etc.
- better results and fewer life disruptions for the same amount of effort
- T1D is still a lot of work, but I more often get to choose when to put in the work, and I get even better results than I did before.
- the ability to program boluses in the future
- I always wanted this with unconnected pumps. I tried my best to make do with extended/dual wave boluses, but those boluses still tended to front-load insulin that I knew I wouldn’t need until some time later when the fat or protein started to hit, or the carbs finally broke through the fibre. Being able to program future carbs makes it so much easier to deal with food that digests more slowly due to high amounts of fibre, protein, and/or fat.
I started with Loop because I was already using an iPhone and that’s the system that ran most easily on iPhones. It is possible to loop with other devices, too, and if I had been using an Android phone at the time, I probably would have started with a system that runs on Android. Here’s a good write-up with links to the various systems out there if you are interested.
Looping is not magic. I’m still using exogenous insulin, and I still can’t take it out once it has gone in, but it’s still light years better than before.
Matching Insulin & Food
Shorter version: Learning to better match insulin to food has meant learning more about how my body digests different foods, and how different insulin patterns cover or swamp the blood glucose effects. My best approach for this has been to keep notes, because I have too many other things taking up space in my head to remember things like this. Learning to better match food to insulin has typically meant eating more fibre and/or protein. In some circumstances (e.g., traveling solo) I use low carb to reduce my margin of error. (next section)
Longer version: I have found that managing T1D is basically balancing food & hormones with insulin & activity. There are lots of things that affect blood sugar (more than the 42 in a well-known list in the T1D community that is missing things like fibre, menopause, etc.), but those four are the biggest ones. A huge part of managing T1D for me is matching insulin and food. This can be done by matching insulin to the food, choosing food that better matches insulin, or a combination of the two. I typically do combinations of both, but sometimes I’ll lean on one or the other. If I am feeling stressed, overwhelmed, or am traveling solo, I am more likely to try to eat food that is more predictable for me (i.e., choose food that better matches insulin). At home or when I’m feeling more up for it, I am more likely to try to figure out how to accurately dose the insulin for a given food.
For me, the key skills for matching insulin to food have been figuring out:
- how much insulin is needed for the food,
- when the insulin will hit,
- when the food will hit and how it will absorb,
and timing the insulin amount(s) accordingly. I mostly do this by keeping notes. I wish I could keep it all in my head but I struggle to extract patterns from vague recollections. I’m much better at being systematic, keeping notes, and adding reminders to recipes & entries in my food log so that the next time I eat that food, I will see my note. One of my favourite notes is on a carrot cake with cream cheese icing we often make for birthdays. My note to self, scribbled at the bottom of the page in my recipe book one day after one of my kids’ birthdays, says: “BOLUS MORE THAN YOU THINK.”
For me, the key skills for choosing food that better matches insulin have been:
- figuring out which foods are more predictable than others, and
- knowing which foods will have a slower (but still predictable) absorption similar to an insulin action curve.
For me, slower absorption usually means more fibre and/or protein. More fat also slows things down, but fat is tricky because it increases insulin resistance and often hits me hard later, so I don’t usually use fat for this purpose. Slower absorption may also mean fewer carbs, though it’s much more common for me to eat things that are high carb and high fibre, like beans, legumes, etc. I do use low carb as a tool at times. For example, when I am traveling solo for work and want to have a smaller margin of error on a restaurant meal, I’ll often look for fish and vegetables on the menu, because those are often available. Some people choose to use this tool all the time. I think that’s a valid choice, and they should be supported by their health care team. I don’t personally want to eat low carb all the time, but I respect the choice among those who make it.
Mental Health & Stress Management
Shorter version: My best lessons for mental health, stress management, and T1D have been that it helps me enormously to: run a lot, do yoga, spend time outside, connect with others with T1D, and sleep. (next section)
Longer version: T1D is hard for a lot of people. I’ve certainly found it hard–more so at times, less so at other times. As I’ve gone through four decades, I have benefited from new management options and learned things that have allowed me to have an easier time, but the neverendingness of T1D is, uh, neverending, and the energy it takes from me at the most inopportune times is always missed. I once read a paper describing a qualitative study of the experiences of younger adults with T1D and was struck by the following two quotes, especially:
“I don’t think people really understand what’s involved. It’s pretty much on my mind the whole time. There’s no day off from it (Female, 30),” and, “It’s a huge thing. But no one can see it so it’s always there and it’s massive for you but it’s invisible for everybody else (Male, 24).”
Even when I’m doing really well at management–sometimes especially when I’m doing really well at management–I’ve learned that I am better on every level when I make time to do things that help my mental health around T1D. The things that help me the most are:
Running. I really depend on running to feel good. I used to do ok running only a few times a week, but I knew it would be good for me to get that boost more often. Some years ago, I worked up to longer distances, 5-6 times a week. It is such a joyful, meditative part of my life now. I don’t race or run with anyone else (except for my dog sometimes, and my dad when we are in the same place.) Running is just time for me. I’m grateful that it is accessible to me.
Daily (or near-daily) yoga. My eldest kid and I started doing 5-30 minutes of yoga together before bed to help my child several years ago, and this habit turned out to also be really great for me. My current endo had once semi-jokingly written ‘yoga’ on a prescription pad when we were talking about the stress in my life as a new professor with a young family. Although I didn’t fill that prescription immediately, I did remember her recommendation. She was right. My kid and I started by doing a 30-day series from Yoga With Adriene on YouTube, and then we just kept going. The daily habit is really helpful to my mental health.
Getting outside. Spending a longer time outside is better for me, but anything is better than nothing. I can usually manage at least a short bike ride (including commuting to work) or a short walk with a colleague, my husband and/or dog.
Connecting (passively or actively) with others with T1D. When T1D has felt like too much, I initially tried keeping its negative mental health impact to a minimum by avoiding thinking about it. This never worked terribly well for me, so I then tried the opposite approach: spending more time thinking about T1D by connecting with others. This works much better for me. Sometimes this connection is active (mostly online but also sometimes offline) and sometimes it’s passive in the form of reading things written by others with T1D or listening to stories on diabetes podcasts. The passive form really serves my introvert tendencies. It has always been helpful to me to get those reminders that others are also dealing with T1D, working at it, and keeping on.
For anyone in Canada: I didn’t know this would be the case when I started writing this post, but, along with a great team of others with T1D and some supportive researchers, I was able to get some research funding recently to create a way for people managing T1D in Canada (themselves, their child, or another loved one) to connect with others in similar situations, life circumstances, etc. Here’s the press release from JDRF Canada (scroll down to the bottom for my team’s project.) We are in the middle of getting this up and running and plan to launch it in fall 2023.
Sleeping. Sleep was always a challenge for me with T1D, especially given I had so many overnight severe hypos as a kid. Being high at night does not make for good-quality sleep, either. I recall when I was younger feeling so incredibly exhausted and drained when I woke up after a night of difficult BGs. I was able to reduce that a lot as an adult, and in recent years, Loop has helped me turn blood sugar sleep disruptions into very rare events. I am also grateful that my husband is willing to provide overnight backup now. Still, life and work responsibilities sometimes crowd out sleep as a priority. I really notice the negative effects on my mental health (and BGs) if I’ve missed sleep to finish a grant, paper, review, student’s application, and so on. I do my very, very best not to sacrifice sleep these days. Most of the time I succeed.
Oops
Shorter version: I use the word “oops” to help me keep my mistakes in perspective and not beat myself up about them quite so much. (next section)
Longer version: Like a lot of people with T1D, I instinctively take it badly when I mess up. If I mistakenly think that I’ll digest something slowly and it hits me quickly, or vice versa, or I underbolus for fat, or I overbolus before a run, or I ignore a pending low that turns into a crash, etc. my easiest, first, go-to response is to get upset with myself. Example:
“WTF how am I messing this up after 40 #%^ing years of this #%^?!”
I’ve learned over the years from talking with others, from reading research, and from just plain trial and error that this response is, to put it mildly, unhelpful.
What is much more helpful is to have some self-compassion. The word I use now to try to evoke some self-compassion in myself is the one I used with my kids when they were small and they fell down, spilled something, or the like: “Oops.” For me, “oops,” carries a sense of, “Hmm, this isn’t quite what I wanted, it’s a mistake, and I’m going to keep it in perspective.” It isn’t perfect, and I still sometimes get upset with myself, but it helps.
What using “oops” is really about is changing the stories I tell myself. I’m not going to pretend to myself that mistakes doesn’t matter to me. My BGs are not neutral data, devoid of valence. Perhaps if I’d had health professionals with different styles over the years, I might have a different factory setting. But as a T1D child of the 80s, I see my numbers as ranging from “good” to “bad.” We can call them “in range” and “out of range,” but I interpret “in range” as good and “out of range” as bad, so changing the words doesn’t change the meaning for me.
Put another way, in theory, I love the idea of seeing my BGs as just neutral data. (And in theory, theory and practice are the same!) But in my real, messy life, I do see my BGs as assessments of how well or poorly I’m doing. I have never been able to talk myself out of this. After trying and failing to shift my reactions, I instead decided to give up and focus on what I can control: the stories I tell myself about what it means. When I say or think, “oops,” I am telling myself the story: ok, this is not what I’d prefer, but neither is it the end of the world.
Outdoors
Shorter version: I have an easier time spending time outdoors when I give a bit of thought to how to keep my diabetes gear and my hands, which I need to manipulate said gear, dry in wet conditions and warm in cold conditions. (next section)
Longer version: I love being outdoors. Spending time outdoors with T1D is easier when I give some thought to how to keep equipment, extremities, and medication dry and at a reasonable temperature. Some things I have found useful that were recommended to me by others dealing with similar issues:
Keeping things dry: In addition to using dry bags when hiking, I use an Aquapac case for my old Medtronic tubed insulin pump when canoeing, kayaking, or spending a lot of time around water. Note that it can reduce flow, so it’s important to keep an eye on that. (Not needing such a case is one of the big advantages of patch pumps, in my view. But the fact that they stay on for 3 days and you can’t go in a sauna is a real turn-off for me, on top of the fact that they are not funded for me where I live.)
Keeping things warm: Canadian-level cold is challenging to electronics (especially glucometers and phones), insulin, and fingertips. I haven’t slept outdoors in winter in a long time but when I was younger, I did things like go winter camping in Saskatchewan with the outdoors club at my high school. (I loved that club so much.) The temperatures went down to -30degC or -40degC at night. At that time, I kept my insulin and meter tucked into my clothes. These days, I’m never out for more than a day. I can get through a day by keeping insulin pump tubing and my spare insulin tucked in a pocket or bra next to my skin. My phone and spare battery go in an insulated pocket in my coat. I used to use hot packs in my mittens, but my Raynaud’s-affected fingertips now get special treatment with these Motion Heat gloves. They are extremely non-free, but have absolutely saved my ability to enjoy winter.
Parenting
Shorter version: Hypo treatments are mom’s medicine; they are not for sharing. I should have stuck to this. (next section)
Longer version: At least when I was pregnant, there seemed a fair amount of medical information available about how to safely have a pregnancy with pre-existing diabetes. But there was almost nothing about how to deal with situations like, “you’re nursing your baby to sleep, which makes your blood sugar drop, and then your CGM alarms right as the baby is dropping off,” or, “your toddler is tantruming and you need to bolus,” or, “you need to drive your kid somewhere on time and you are too low to safely drive.” My kids are 16 and 11 now (fortunately for them and us, neither one has any health issues, despite my multiple autoimmune conditions) and my T1D has definitely influenced my parenting occasionally. Some things I have learned over the years about parenting when the parent has T1D:
Breastfeeding an infant decreased my insulin needs by about the same amount as hiking all day. I needed about about 60% of normal basal, no change in insulin-to-carb ratio. Breastfeeding a toddler decreased my insulin needs slightly, but not nearly as much as when I was the sole source of food. Having a pre-established hiking basal pattern really came in handy when I had nursing babies and toddlers. Still, stashing low snacks anywhere I might nurse was always a good idea.
I should not have let my children try glucose tabs when they were toddlers. I thought that if I let them taste the chalkiness of tabs, they’d never ask to share them again. That was a mistake. I am embarrassed that I made the same mistake twice.
Once kids can speak clearly and know their numbers, they can learn to dial 911 and tell the operator, “my mom is sick and she won’t wake up.” Fortunately neither one ever had to do that, but we taught them how, occasionally practiced, and kept a landline for that purpose.
Once my children were about 4 or 5, it was helpful to teach them to please try not to ask me questions when I’m low. My decision-making capacity completely vanishes when I’m hypo. They don’t always remember, but then, no one always does, not even adults. Knowing that it’s a thing, though, if I say, “I’m sorry, I can’t answer right now, I’m low,” they understand a bit more about what is happening and can be patient, knowing I will be able to answer soon.
As my kids have grown, I think (hope?) it has helped as I have voiced more of what’s going on for me with my T1D, including giving voice to my emotions around T1D and how I am dealing with them. I hope I am modeling good habits.
I think it might help children have more empathy when they grow up with a parent with a chronic illness.
It’s really hard but really important to put on my own oxygen mask first. I need to stop and make sure I am bolusing correctly, even if it means a child has to wait. Taking care of myself means I can continue to be there for my kids long-term.
Perimenopause
Shorter version: AAAAAAARRRGGGGHHHH. The best I’ve got at this point is: staying flexible and being as serene as I can about unpredictability helps somewhat. I also find it really helpful to do more sprinting and heavier strength work. (next section)
Longer version: My insulin sensitivity has always changed with my cycle. The changes are not as dramatic as they are for some other people, but they are enough that I’ve always needed more insulin in the days leading up to the start of my cycle, and then much less insulin in the days after my cycle starts. I learned in recent years that I had not properly appreciated the formerly predictable nature of my cycle. Now that I am firmly in the years of, “Will it be 14 days between cycles this time, or 73? Is my site going bad or am I having wildly fluctuating hormones today?” I miss that predictability very much. I wish I could write that I have learned how to handle perimenopause expertly and here’s what I have found, but all I’ve really learned is to be even more flexible and agile with my management. It reminds me of pregnancy in that way. I don’t wait for a pattern to be really solid before I make an adjustment. If it seems like my body needs more insulin today, I assume that something hormonal is going on and crank up all my ratios by at least 15%. Same thing if I seem to need less insulin: I just dial it down by 15% or more and see if that settles things down. If not, I adjust up or down according to what I am seeing. It is a constant guessing game. I just do my best.
I’m still in the middle of perimenopause, so I hope to have more lessons learned in a few years. I will say that living with T1D for decades prepared me reasonably well for the experience of having things that used to work great for me no longer working so well, and also for having my body need my attention and behave in unpredictable or unwanted ways. I think it’s always tough the first time you realize that your body may not be as reliable as you’d like, and although I would 100% trade places if given the option, I do recognize that living all my life with a chronic illness prepared me somewhat better for managing other issues than people who have been generally healthy all their lives.
They are not T1D-specific, but I’ve found the book Next Level and associated podcast Hit Play Not Pause to be useful for general perimenopause and health information, especially regarding physical activity during perimenopause & menopause. (See also section Podcasts if you want to know my T1D-specific favourites.) I struggle a bit with the ads extolling the virtues of CGM for pancreatypical people, but I am trying to get over myself, and enough of the sports information has been useful to me that it’s worth that minor annoyance. (It’s probably good practice for me to get over myself there so I can apply that skill in other domains, too.) Among other things I’ve learned, after focussing on increasing kilometres in recent years, I have now re-balanced my focus so I’m doing more strength training and sprints. I really, really like short sprints, so this is extremely fun. Also, although my running kilometres have decreased a bit, I’m getting faster again. I mainly run for mental health, but I also like feeling like I’m improving.
Physical Activity (Exercise)
Shorter version: Being active is great for my T1D overall, partly because of direct effects (increased insulin sensitivity) and partly because of indirect effects (better mood, easier time eating well.) It is not always easy to fit into a busy life, though, especially when I want to avoid hypos during exercise. I find it helpful to understand how different types of activity influence my BGs. Here is some official guidance about exercise and T1D. I don’t use all of the recommendations (see next section for more on exercising with insulin on board) but I think it’s a great starting point. (next section)
Longer version: Physical activity is intensely good for physical and mental health, and it is my favourite stress management strategy. I’ve always liked it. I played field sports in high school and university, then my husband and I met playing one of those field sports (at a very appropriately-named ‘pick-up’ game.) We incorporated a game with our teammates, family and friends into our wedding, and spent our honeymoon at nationals. I stopped playing competitive sports when I had babies, but I remained active, with the level of activity varying with the ages of my kids and the stage of my career. My level of activity was high when I was playing competitive sports, went down when I had young children and my work was also demanding a lot of my time, then went up again as my kids got older and I got better at delegating at work.
Overall, physical activity helps with my T1D, partly because of the direct effects of exercise on blood sugar, and partly because I just naturally eat better when I’m more active. But fitting activity into my busy life with T1D, an intense job, and two kids requires trial, error, and compromises. These days, my kids are 16 and 11, and I run about 45-50 km a week (mostly outdoors, year-round, though I use a treadmill if it’s too slippery and/or dark out), strength train twice a week, do yoga with my 16-year-old most nights, take walks with my husband and 11-year-old most weekdays, and mix in other fun things like swimming, bicycling, cross-country skiing, snowshoeing, and hiking.
I have not run continuously all my adulthood. When I’ve wanted to come back from an injury, pregnancy, or I’m-barely-sleeping-due-work-pressures-how-can-I-possibly-run break, I used to start with a couch to 5k program and remind myself that it typically takes me 4-8 weeks of running regularly to start enjoying it again. I was always a bit prone to injury, though, especially shin splints, so the last time I restarted, I found a (re)start running program that includes a focus on injury prevention, called None To Run. I started with the free trial (it’s been a while but if memory serves, I got a week for free to try it out) then paid for the app. It was worth it for me and got me back into happily running. From that point on, I made it a mental health priority, made sure to keep doing strength and flexibility work to avoid injury, and (touch wood) haven’t had any problems. Once I was running 3 days a week again, I deliberately lost some weight to make it easier for me to add more running days (see section: Weight Management), increased the length of my runs and added more running days, typically limiting the addition to 10% per week, until I got to my current happy place of 45-50 km/week over 5-6 days a week.
The main lessons I have learned over the past 40 years related to physical activity with T1D have been:
- It’s easier BG-wise to exercise with minimal insulin on board (IOB) but it’s possible to fit exercise into my life rather than contorting my life around exercise. (See Physical Activity with IOB below.)
- There’s a spectrum between aerobic/endurance activities (e.g., running) and anaerobic/power activities (e.g., weight lifting.) The effects of activity on blood sugar are different along that spectrum. Aerobic/endurance activities are more likely to reduce blood sugar while anaerobic/power activities can increase it.
- Things that I wouldn’t have classified as exercise when I was young and naive are still physical activity and impact me the same as exercise. For example, I had never thought of gardening as exercise, but between the constant movement, digging, lifting, and so on, it turns out it’s about the same as walking for me.
- Hypos during exercise are annoying, but they are not the end of the world. I avoid them as best as I can, and I’m reasonably successful at that. (See the next section for more on that.) On the occasion when one happens anyway, I treat the hypo and keep going if I can. Accepting them as occasional disruptions and not getting too upset about them has been important for me.
For anyone who wants to read more from official perspectives, here is some official guidance about exercise and T1D and a recent paper (both led by Mike Riddell, a scientist with T1D.) I also found Sheri Colberg’s book really helpful when I found it in the early 2000s. Here is her more recent book, which I have not yet read. I also recently saw that there’s a new book out by Ginger Vieira, which I haven’t read, either, but it looks really interesting.
Physical Activity (Exercise) with Insulin on Board (IOB)
Shorter version: I think some of the advice given around exercise (e.g., hammering how important it is to exercise with little to no insulin on board) makes it more difficult to fit exercise into a busy life. I have found it possible to exercise with IOB by accounting for the fact that IOB will be multiplied by 3 on average during activity and adjusting insulin and timing of food and activity accordingly. Spontaneous exercise is still harder to manage than planned exercise, because I have to balance out any IOB with some fast carbs before starting, but it is possible. If I can plan a little and I know I am going to be active after eating, I typically reduce the total bolus and increase prebolus time. The longer prebolus blunts any initial spike. The reduced amount helps avoid excessive IOB. (next section)
Longer version: Many people with T1D recommend exercising fasted (i.e., with no insulin on board, IOB.) I agree that this is easier. There’s less to consider. I do this some of the time, especially when I only have time for a short morning run and am willing to forgo morning coffee before running. However, this may not be ideal for perimenopausal women, and also, it would be extremely limiting to my life to restrict myself to never exercising with IOB. I don’t want to limit myself that way, so over time, I have figured out how to use insulin under conditions of physical activity, bringing a lot more flexibility and enjoyment to my life.
Insulins like Fiasp (my current insulin), Humalog, NovoRapid/Novolog (my former insulins), etc. typically last 4-6 hours. Most of the insulin is used up after about 4 hours, but a small amount remains until about 5-6 hours out. This is what the scientific literature says, and my own experiences match the literature. Therefore, for me, avoiding exercising with any IOB is often impossible or undesirable. For example, I lack the desire or ability to fast for 5-6 hours prior to:
- playing 3-4 matches per day at a 2- to 4-day tournament
- going for a walk after lunch
- running 20-25 km on my weekly long run
- hiking all day to get to the next campsite
- swimming laps after supper because that’s when I can get to the pool
- doing strength training after supper while my kid is in a lesson at the same facility
To deal with these kinds of situations, I have spent a fair amount of time and effort over the years figuring out how to exercise with food and insulin on board.
The key things I have learned are as follows.
If I am moving gently but consistently for a long time (walking, gardening, paddling or hiking all day), getting my heart rate up for a sustained period of time (running, bicycling, swimming, cross-country skiing, snowshoeing) or getting my heart rate up in intervals (playing a competitive field sport, running sprints, high intensity interval training), whatever insulin I have on board (IOB) will behave as if it has been multiplied by 3X on average. This (3X) is the default average I assume for new activities, but I track and refine over time the actual multiplier for repeated activities. For example, some of my current multipliers that seem to be working for me these days are:
- bicycling (slowly, for pleasure, <1 hour): about 1.3X IOB
- bicycling (slowly, for pleasure, >1 hour): about 1.5X IOB
- bicycling (moderate pace, for transport): about 3X IOB
- cross-country skiing (leisurely pace with kids & occasional stops, <2 hours): about 2X IOB
- cross-country skiing (moderate pace, at least an hour or two): about 4X IOB
- gardening: about 2X IOB
- running (easy <10km, no sprints): about 4X IOB
- running (moderate <10km; easy >10km, no sprints; speedwork of any length): about 5-6X IOB
- soccer/field sports: about 3-4X IOB
- swimming laps (moderate effort, long breaks): about 3X IOB
- swimming laps (moderate effort, no long breaks; sprints at the end): about 4-5X IOB
- walking: about 2X IOB
- yoga (gentle): about 1.2X IOB
- yoga (lots of planks, etc.): about 3X IOB
As I understand it, insulin on board acts as if it has multiplied itself during aerobic activity because, during exercise like walking, running, etc.:
- muscles are sucking up some of the glucose directly without requiring insulin to open up the cells,
- insulin receptors bind to insulin more efficiently than usual, meaning it takes less insulin to open up the cells to glucose, and
- digestion slows down, so anything I ate beforehand is not hitting at the same rate it typically would.
- Stomach to brain: “Hey, brain, I see we are running, uh, maybe from a bear? How about I just send some of my energy to the heart, lungs, and leg muscles? This meal will still be here to digest later.”
When I need or want to exercise with IOB, I can either:
- reduce insulin ahead of time according to my multiplier (this requires not waiting too long after eating to start moving, or I’ll spike)
- add some carbs up front or during the activity to balance out the excess insulin (using the correct multiplier), or
- a combination of both approaches.
Below is an example of what my approach looks like for a 2-hour run. (The shorter run version is more or less the same, just with less time spent running. I don’t always eat before a short run, but I do prefer to have something in my stomach before heading out, especially for winter running, so this is my approach the majority of the time.) This is a typical weekly long run for me, done on a weekend day. In winter in Quebec City, I want to be outside at the warmer part of the day, so I try to run starting around 10:30 or 11 a.m. In summer, I do the opposite and aim to leave earlier. I’m using Fiasp, so the time between bolusing and eating is shorter than it used to be when I used NovoRapid. Note that typically, my prebolus time for Fiasp is about 10-12 minutes. Here, for the oatmeal, I used a much smaller amount but gave it 30 minutes in advance. (This is what I wrote above about how my typical approach is to use much less insulin, but give it further in advance.) On this day, I followed my usual loose routine:
- 9:30 a.m. bolus 0.7U to cover coffee with lots of milk (total 12g CHO from the milk, and 6g fake carbs for the caffeine)
- 9:40 a.m. drink coffee, read a paper
- 10 a.m. bolus 0.3U to cover 1/3c oatmeal with 1t milk powder, 20g raisins, 1T ground flaxseed, 10g chia seeds and 1t maple syrup (total 46g CHO, 9g fibre); turn on 3-hour 15% override (meaning Loop will be giving me only 15% of whatever insulin I would normally need for the next 3 hours); get dressed in layers upon layers to run in the cold, make sure I have glucose gels, spare phone battery, emergency hand warmers, ice spikes, etc. ready to go
- 10:30 a.m. eat oatmeal, double-check I have everything I need
- 10:50 a.m. start running
- about 12:30 p.m. take a glucose gel (26g CHO) because I didn’t think my BG was going to hold all the way home
Note: I have my low threshold set at 4.2 mmol/L (76 mg/dl). The parts of the graph where the line is touching the top of the pink section are actually still in range, i.e., 3.9 mmol/L (70 mg/dl) or higher.
I really like to be around 4.2-5.0 mmol/L (76-90 mg/dl) when I’m running. I feel absolutely fantastic and energetic at a flat 4.2 (it’s my favourite BG for how it makes me feel energywise) so it was important to me to figure out how to do this.
My non-oatmeal favourite breakfast before a run is 1-2 small slices whole wheat raisin bread with peanut butter, sliced banana, and cinnamon. (I swear, if cinnamon cured diabetes, I would not need to write this post.) This beloved breakfast is an option when I’ve made the bread, using my Oma’s recipe that my uncle and godfather adapted to whole wheat. If I have 2 slices, it takes about 0.5U rather than 0.3U. In other words, on those days, I take 1.2U (0.7U for coffee and milk, 0.5U for food) for about 100g total of carbs. This is roughly 6 times less insulin than my body would typically need for this breakfast, which aligns with my point above about how running multiplies IOB by about 5-6X on a long run. It is exactly the right amount of insulin for this food before a long run. I am moving the whole time and I feel fantastic.
When I come back from a run, I switch off the 15% override and see if Loop suggests a bolus. If it does, I usually give that bolus. If it doesn’t, I will still typically take about 0.5U because I know that as my digestion picks back up, my stomach is going to start sending more oatmeal/raisin bread glucose to my cells and it will be good to have those cells open to receive the glucose.
If I think I might spike a bit post-run due to adrenaline, a recent glucose gel, or just a feeling that a spike is waiting to pounce when my digestion picks back up, when I get home, I will often bolus and then take my dog for a quick walk. The walk helps the post-run bolus kick in quickly, and walking after a hard run can tamp down the adrenaline that can otherwise push my BG up. It also helps my dog feel less sad after being left behind. He comes with me for shorter runs but is not focused enough for 2+ hours of running. (Squirrel!!)
If I’m heading out to do something active and I just don’t think I have quite enough carbs on board to balance out the insulin, I will use one of two approaches to balance out the extra IOB:
- The more portable, can-do-this-anywhere approach: Take some glucose tabs or drink some Gatorade about 5-10 minutes before starting. I mostly use this approach if I am going somewhere else to exercise, like walking to the swimming pool or driving to a hiking or cross-country ski location.
- The more enjoyable, can-really-only-do-this-at-home approach: Put some nut butter on a spoon, add ~10g honey from a squeeze bottle on top, then quickly flip the spoon upside down in my mouth, with the honey next to my tongue. I mostly use this approach if I am leaving directly from home to go running, cross-country skiing or snowshoeing near home. The honey isn’t as quick as glucose tabs but is usually fast enough to provide an immediate glucose bump, and putting it right next to my tongue and cheek may help it hit a bit faster. The fat in the peanut butter helps stretch out the honey’s impact and may slightly lower my insulin sensitivity, which I want while I’m active. Also, this is incredibly delicious if you like peanut butter and honey, which I do. (Since I live in Quebec, home of the world’s global strategic maple syrup reserve and producer of 75% of the world’s maple syrup, I once tried this with maple syrup. It was not a good mix. I now stick with honey.)
If I am doing a power activity (strength training), it’s a different situation. Many people with T1D report needing to take insulin to lift weights. When I did heavy lifting as part of a required training program for very competitive sports, I did not need to take insulin to balance that out, but I usually met a teammate at the gym in the afternoon (hi, Diane!) so my lunch IOB may have been doing some heavy lifting (ha) there. I do find that I rarely go low while strength training unless I get a bit too enthusiastic about warming up on the treadmill. I also find that lifting heavier weights (e.g., doing 5×5 with a heavier weight rather than 3×10 with a lighter weight) seems more likely to drive my BG up. I also find that I seem to be a little insulin-resistant for about 8 hours after heavy strength training, and then my sensitivity shoots right up again.
These days, I am strength training at a facility while my youngest is in a 2-hour program at that same facility. My kid’s activity runs after supper one night a week and after breakfast one morning a week, and I start and end each strength training session with some short cardio (10-20 minutes of running or time on the one and only erg, which I have used in a nod to the year I spent rowing in my teens, first on an erg, then bicycling to Wascana Lake at dawn.) The best approach I’ve found in this case is to back off on my insulin (basal and meal bolus) by about 50% leading up to strength training (starting about 2 hours ahead) and set a higher target (6.3 mmol/L, 113 mg/dl) so that I can get through the cardio and the first 20 or so minutes of the workout without going low. But once I start the workout, as the time goes on, that insulin deficit starts to hit me along with any effects of strength training, and then I may need to balance out the deficit by adding insulin. Thus far I’ve been doing that with a 150% override rather than a bolus, because I need to be ready to receive my kid when the activity is over and don’t want to risk a low, but I suspect the more accurate approach would be a small bolus of insulin. Another approach that has worked well on the occasions I’ve tried it was when my husband took our kid home and I ran home–no insulin needed as a result. I’m still experimenting with the best approach for this.
In summary, yes, it’s easier to exercise with no IOB, but by figuring out how different activities multiply IOB, I have brought more flexibility into my life. I hope that others who want more flexibility may find this idea useful, too.
Podcasts
Shorter version: I find it helpful for my T1D management to include T1D management-oriented podcasts as part of my regular podcast feed. My two favourite such podcasts are Juicebox and Insuleoin. (next section)
Longer version: I like podcasts because I can listen while doing something else (e.g., cooking, cleaning, weeding the garden, changing my set, running.) I have an eclectic mix of podcasts I regularly listen to, including some that are diabetes-specific. I really dove into diabetes podcasts during the first two years of the Covid-19 pandemic, when I found it difficult and overwhelming to listen to former favourite podcasts about science, current events, and health research.
It’s surprisingly rare on T1D-focused podcasts to get into the nitty gritty of how people plan a bolus or deal with a situation, and yet, that’s what I want. I want the numbers and the specific examples. I know that what worked for someone else may not work exactly the same for me, but hearing the specifics of what they did helps me map ideas that might be useful to me. There are two T1D-specific management-oriented podcasts that I especially like: Juicebox and Insuleoin.
What I like about this podcast:
- Tons of content, lots of it helpful. The in-depth conversations about the specifics of management are really great. Sometimes get new ideas, but even if I don’t, the reminder/time to reflect on a given issue is useful.
- I love the interviews/stories because they provide a low-effort-required way to remind myself that lots of people are working hard at T1D and often living very well with T1D.
- Promotes a good, pragmatic attitude about T1D.
- No pre-recorded ads played over and over again. It’s one of the few podcasts where I usually let the ads run and listen to them rather than skipping ahead.
- Interviewees are extremely varied. I love the different lives and experiences people have had. I especially like the interviews with kids and with older adults, especially older women who have lived with T1D longer than I have.
- Host is kind to interviewees, and often very funny.
- The episodes with diabetes educator Jennifer Smith are the best. She’s fantastic and I love her accent. (Once, I was listening to Q&A episodes while doing some light post-run strength work. I decided I’d do 10 push-ups every time she said, “and what not,” in her charming accent. I did 140 push-ups that day.)
- In addition to the management-focused episodes, I’ve also picked up management ideas from the story episodes. For example, there was an episode with a dentist who suggested keeping water by your bed so that if you treat a low in the night and just can’t bring yourself to get out of bed and brush your teeth again, you can at least swish water over your teeth, which may even be better for your teeth than immediately brushing. I’ve done that ever since. It also helps me drink water first thing in the morning.
- The great protips series helped me a ton when I hit perimenopause and needed to make a bunch of adjustments. I already knew what to do, but I was exhausted and didn’t want to put in the effort that I knew I needed to put in. The protips series gave me a structure to systematically work through, and it reminded me that lots of people work hard at diabetes. I felt less alone, and that was really valuable to me.
- My husband listens to this podcast. He doesn’t enjoy any of the other diabetes podcasts that I like. (I am really touched that he listens to a diabetes podcast regularly.) I think listening to this has given him extra insight. A few months after he started listening, he came to me, referenced my Dexcom graph on his Follow app, and said something like, “Hey, I just want you to know that I see how much work you’re putting in that no one sees.” No one had ever said anything like that to me, and it was incredibly meaningful to me. I cried.
Caveats:
- There’s relatively little information about exercise, and what exists can be limiting. I wish Scott (the host) would make better use of Jennifer Smith’s (diabetes educator who was already known in the T1D community for her depth of knowledge on exercise and nutrition) experience with exercise. An actual one-sided conversation that happened as I listened while out on a long run with 1.2U of insulin on board to cover ~100g carbs: Scott, in my ear: “I think you just shouldn’t exercise with active insulin.” Me, out loud, startling a guy walking by: “[bleep] you, Scott, how about I just don’t live my life, then?”
- The podcast occasionally veers into woo of late. This is mostly kept in check, so it isn’t a major problem, but I notice my antennae going up from time to time. My childhood history with a supplement-enthusiast mom who encouraged mantras while not taking me to an endo puts me on guard against woo, so I may be hypersensitive to this. I do not see this as a major problem in this podcast.
Some of my personal favourite episodes/series:
- The whole T1D protips series (note that there’s a new protips series starting up on T2D, which I think is a great idea that may prove useful to people with type 2 diabetes)
- “Ask Scott and Jenny” episodes (just maybe don’t commit to doing 10 pushups every time Jenny says “and what not” … or do, if you want a good upper body and core workout)
- The variables series
- The three “Fox in the Loop House” episodes (#312, 313, and 420)
- Probably my favourite episode was How We Eat: Vegan Cat, just because it was so funny. I listened to it while running and nearly fell over.
- I also loved the interview with Alisa Weilerstein, a professional cellist. It was a great story and the podcast played her recording of the Prélude of Bach’s Cello Suite No. 1 in G Major, a gorgeous piece of music that she plays beautifully. I heard this one while running along the St. Lawrence River in the rain on a drizzly Saturday and it was so, so lovely. I bought the whole album when I got home.
What I like about this podcast:
- It has an intense focus on exercise, so there’s a lot of content that is useful/relevant to me.
- I really like some of the ideas about how to think about diabetes. After living with it for so many years, it’s easy to fall into thought patterns that may not be ideal, so I’ve found it helpful to consider new ideas and approaches. One idea I found particularly useful was to think of high or low BGs as an opportunity to practice how I respond both practically (how do I manage the high/low with insulin, food, activity, etc.) and emotionally (how do I avoid beating myself up.)
- I love the host’s Irish accent. It’s an especially nice change since so many other English-language podcasts are from the US.
- I like the dynamic between the host (Eoin) and producer (Graham). They are funny together and having a producer involved who does radio professionally brings a level of expertise.
Caveats:
- The host, Eoin, has never used a pump and doesn’t talk about how to use pump functionalities like reducing basal ahead of exercise.
- There’s a real Instagram vibe to this podcast. I imagine that works well for people who are active on Instagram. It’s just less enjoyable for me. I tend to skip over the one-influencer-interviewing-another episodes, but there are lots of other episodes that I like.
Some of my personal favourite episodes/series:
- The series about different types of exercise:
- #22: Hypo Anxiety with Danny Gallagher was a great interview overall and I especially liked the discussion about BGs and mood
- #72: Fulfilling an Olympic Dream with Alan Sothern was one of my favourite interviews
- #105: Why Am I Annoyed? had some useful ideas about how to deal with BG excursions
- #117: What Do You Want From Your Diabetes had some good food for thought (I had never asked myself those questions before)
- #141: Bursting Through A Trampoline & Breaking Both Legs, World Diabetes Day had some discussion of attitude & positivity that I liked
Other diabetes podcasts I listen to regularly, meaning I listen to most episodes. Some are more management-focused, others are more story-focused:
- Diabetes Canada
- I am admittedly biased because I have done some work with the host, Krista Lamb, and I know a lot of the interviewees. But some of the episodes have been really instructive to me; for example, I especially liked Season 7, Episode 1 with Jane Yardley discussing her research on T1D, exercise, and particular considerations for women.
- Diabetes Connections
- The host of this podcast, Stacey Simms, is the mom of a kid with T1D and used to be in radio news. The podcast is really well produced, very professional, I love the summaries of news & science, and the host does an excellent job of interviewing device manufacturers.
- Taking Control Of Your Diabetes
- This podcast is by two physicians who have T1D themselves. This one is more management-focused, but is pretty 101-level. I don’t love every episode, but I rarely skip one, and I do sometimes get useful ideas.
- Talking Type 1
- I really like the stories on this podcast, and the host, Dan, is extremely thoughtful and skilled at interviewing people about their experiences, including topics that can be difficult.
Other diabetes podcasts I listen to occasionally and have enjoyed:
Prebolusing
Shorter version: Digestion is often faster than insulin. Back in the day with older insulins, I used to have to give insulin 45 minutes to an hour ahead of time. Even now, with faster insulins, if I want my insulin to match my food, the insulin still needs a bit of a head start. Apparently we now call this a prebolus. I use a 10-12 minute prebolus for Fiasp. When I used NovoRapid/Novolog, my prebolus time was typically 30 minutes, hence my enthusiasm to move to Fiasp. (next section)
Longer version: It was honestly a surprise to me when I learned that (a) some people with T1D don’t know to give the insulin a bit of time to start working before eating and (b) this is such a thing that it now has a name, “prebolusing.” When I was first diagnosed and used two daily injections of slow (NPH) and fast-acting (Regular) insulin with a strict meal plan, the instructions were to give insulin 45-60 minutes before breakfast and supper. So prebolusing was just giving the insulin when they told me to. I have many memories of jabbing myself with my insulin pen while waiting in a long lunch line at the cafeteria in university, and hoping that the carb count I was guessing would be achievable with whatever was on the menu. I repeated a lot of salad and sandwich bar staples, because I knew I could count on them being there. No one else liked the whole wheat buns, I guess.
As insulins got faster, that time got shorter, but it has never been zero minutes unless the meal was something that would be really slow to hit. Even with Fiasp, I get better results with a small prebolus, typically 10-12 minutes. I understand that people in places with access to inhaled insulin may be able to take that right as they eat, but I have never had access to that here in Canada.
Figuring out the right prebolus time for me has been a matter of trying out different timing and watching my graph.
If I can’t prebolus for some reason, other ways I’ve learned to help the insulin match the food for me are:
- eat fewer carbs,
- eat the protein, fat and/or fibre before the carbs,
- eat more slowly,
- wait, while sipping a drink or picking at the food,
- add an hour or two of basal to the bolus, then turn off basal for that amount of time (John Walsh calls this a “superbolus” in the book Pumping Insulin), and/or
- get some activity after eating, like a walk, bike ride, or a quick set of squats after lunch. (See Highs & Spikes for more on this.)
An important concept for me for prebolusing is that I am trying to match insulin to food absorption. (See also: Matching Insulin & Food.) This means the timing—while relatively similar for most meals—may need to be tailored to the food. For foods that are likely to hit harder as they start to digest (e.g., cold cereal, a sandwich, normal pasta) I often need more of the insulin front-loaded. In other words, I need more of the insulin to be already working by the time my body starts to digest the food. In these situations, it helps me to prebolus longer. Even getting part of the bolus in well ahead of time helps. That is sometimes all I can do if I’m on the low end. This is one of the great things about a pump. It’s really easy to put in some insulin early and then more later. Breaking up my boluses like that has always been useful when I’m uncertain about the meal; for example, at restaurants, cafeterias, potlucks, etc.
Pregnancy & Breastfeeding
Shorter version: The big challenge of pregnancy and breastfeeding is keeping on top of how insulin sensitivity/resistance changes with changing hormones and activity. It’s doable, but hard work. I love my kids and they were totally worth the effort. I have heard good things about this book as a resource. (next section)
Longer version: My pregnancy and breastfeeding experiences are long in the background of my life now that my kids are 16 and 11, but for anyone for whom it might be useful, the most helpful management-oriented things I learned about pregnancy and breastfeeding with T1D that I didn’t see discussed much by others at the time were as follows.
HbA1c automatically drops by about half a percentage point (6 mmol/mol) during pregnancy due to increased blood volume. This means that a reduction in HbA1c from, for example, 6.5% to 6.0%, doesn’t necessarily reflect changes in my T1D management, and I probably need to do more if I want to get that number lower.
It is common to have reduced insulin needs around the end of the first trimester, so watch out for that. (Memories of waking to a bunch of first responders and an IV in my arm at 14 weeks pregnant with my first kid … our housemate never forgave us for not waking him up to enjoy the houseful of firefighters.)
I made a chart of insulin needs for each pregnancy. For my first pregnancy, this involved correctly guessing the password to the password-protected pump database. Many thanks to the engineer at Deltec who gave me a great, broad hint on the phone about trying obvious terms. (The password was “Deltec.”) For my second pregnancy, I mapped insulin needs by week of pregnancy against the first. I’ve shared this before in various places, including with the endocrinologist I saw for my second pregnancy. She also saw my Dexcom reports. Eighteen months later, she went on to lead CONCEPTT, the international trial that found that continuous glucose monitors were helpful in pregnancy.
Exercise makes it easier to cope with morning sickness that lasts all the way through 9 months, making it easier to manage blood sugar. (Memories of my second pregnancy, when I was a regular at our local swimming pool’s evening lane swim…)
It’s OK to choose to ride a bike while extremely pregnant. It was great for my T1D management and my overall happiness. Many thanks to the (Dutch) maternal-fetal medicine doc who explained to the (not Dutch, and extremely alarmed) fellow that people do it in the Netherlands all the time, and that I am capable of assessing the risks and benefits and deciding the benefits are worth the risks. (I will always remember biking to an appointment at 40+5 weeks pregnant, then showing up two days later at 40+7 to have the baby in an uncomplicated VBAC, or vaginal birth after cesarean.)
Some years ago, I provided answers to questions for what ultimately became this book by Ginger Vieira and Jennifer Smith about pregnancy and T1D. I have no idea if my answers were used, as the book came out after I had my babies and I haven’t taken the chance to read it. I’ve heard great things about it, though, and know enough about their qualifications to assume that it’s likely a great resource for people with T1D who are planning a pregnancy or already pregnant.
I will add here now with the benefit of nearly 17 years of perspective that all the effort was completely worth it. I feel that even more strongly now that my kids are much older. I loved my years with babies and little kids, but I find parenting older kids even more interesting and fun.
Protein & Fat
Shorter version: I’ve tried a lot of approaches over the years for bolusing insulin with protein and fat in mind. What I’ve found to work best for me is a 3-step process for any larger (>500 calories) meal: 1) bolus for carbs 12 minutes before eating, 2) an hour after the meal, bolus for 0.4 x grams of protein as if they were grams of carbs, and 3) 3 hours after the meal, bolus for 0.9 x grams of fat as if they were grams of carbs. This level of attention to detail is unnecessary for smaller meals, where a carb-only bolus is enough for me. (next section)
Longer version: My T1D is easier to manage when I eat more protein than my original exchange meal plans suggested. I currently aim for about 1.6g/kg daily, which means 20-30g per meal/snack across three meals and a snack. It took me a while to get here, and I resisted the idea, because my family doesn’t eat a lot of meat and I had such a bad time when I tried low carb. But it is very clear to me from trying it that making sure I get a good amount of protein definitely helps my blood sugar and makes me feel good. Most of the protein comes from beans, pulses, eggs, Greek yogurt, protein powder when I need something more convenient, and whole grains. (Whole grains can have a surprisingly high protein count if, like me, you’d originally thought of them as pure carbs. Canadian whole wheat flour is required to be at least 13% protein.)
Like many people with T1D, I was taught to bolus only for carbs. I would account for higher-fat (and also higher-fibre) meals by stretching out boluses using combo/dual wave or extended/square wave boluses. I have learned over the years as my management has gotten tighter that things go better when I explicitly bolus for protein and fat. Protein converts to glucose (just more slowly than carbs) and fat increases insulin resistance. I think of fat coating the cells sort of like how sunscreen coats skin. It stops insulin from opening the cells as much as it normally would, so I need more insulin to get through to balance the food.
This write-up for diabetes educators is my favourite resource about bolusing for protein and fat, and I also initially found this blog post about the Warsaw method extremely helpful for structuring my approach. I noted that the Warsaw formula is a function of calories from fat + calories from protein + 2.5 times calories from carbohydrates. Since I have those numbers already in my food app (see section: Logging food), I just draw straight from the meal summary and bolus for one tenth of the calories from protein (grams of protein x 0.4) 1 hour after the carb bolus as if I’d eaten that many grams of carbs, and 3 hours after the carb bolus, I do the same thing with grams of fat x 0.9. Thanks to Loop, I find I only really need to do that for larger meals, meaning anything over about 500 calories. This usually means supper, but sometimes a larger lunch also takes this kind of attention. If it’s really heavy fat (about >20g or >30g), I assume I will need more insulin overall to tackle the insulin resistance, so I sometimes try an override, though more often I just go for a walk.
In other words, I bolus for most larger (>500 calories) meals as follows:
- 12 minutes before eating: bolus for carb grams minus half of the fibre grams
- about 1 hour after eating: bolus for grams of protein x 0.4 as if they were carb grams
- about 3 hours after eating: bolus for grams of fat x 0.9 as if they were carb grams
Example:
As I am writing this, tonight, we had fish in packets with edamame, couscous, a green salad, and baked apples with ice cream for dessert. My father-in-law is visiting, hence 5 servings, but otherwise this is a very typical meal at our house. Here’s what that looked like, how I bolused for it, and how that worked out.
The food:


The meal analysis:
The boluses:
- Shortly before eating: bolus 68g carbs (3h absorption in Loop)
- How I got 68: 74.2g carbs – half of 12.8g fibre = 74.2 – 6.4 = 67.8 = about 68g carbs
- An hour later: bolus 16g carbs for protein (3h absorption in Loop)
- How I got 16g: 40.8g protein x 0.4 = 16.32 = about 16g carbs equivalent for protein
- 3 hours later: bolus 21g carbs for fat (4h absorption in Loop)
- How I got 21g: 23.1g fat x 0.9 = 20.79 = about 21g carbs equivalent for fat
And here’s how it worked out. I messed up the initial part of this (oops) because I had planned to make rice, but I filled the rice cooker and then forgot to turn it on. All we use is brown long grain rice, which takes at least 45 minutes to cook, so I was rushing around making a replacement grain at the last minute (couscous, 5 minutes’ cooking time), which drove me a bit too low pre-meal, and then in my rushing around & cognitive deficit from the low, I forgot to prebolus (oops again.) I knew the meal wouldn’t hit too quickly because I had a salad and a lot of protein to eat, so I just didn’t worry about it and programmed the boluses as I would normally, only without the 10-12 minutes I usually let the insulin get moving before I start eating. I had a rise up to 8.0 mmol/L (144 mg/dl) that I otherwise probably wouldn’t have seen, but that’s fine, and after that, my BGs did exactly what I wanted.
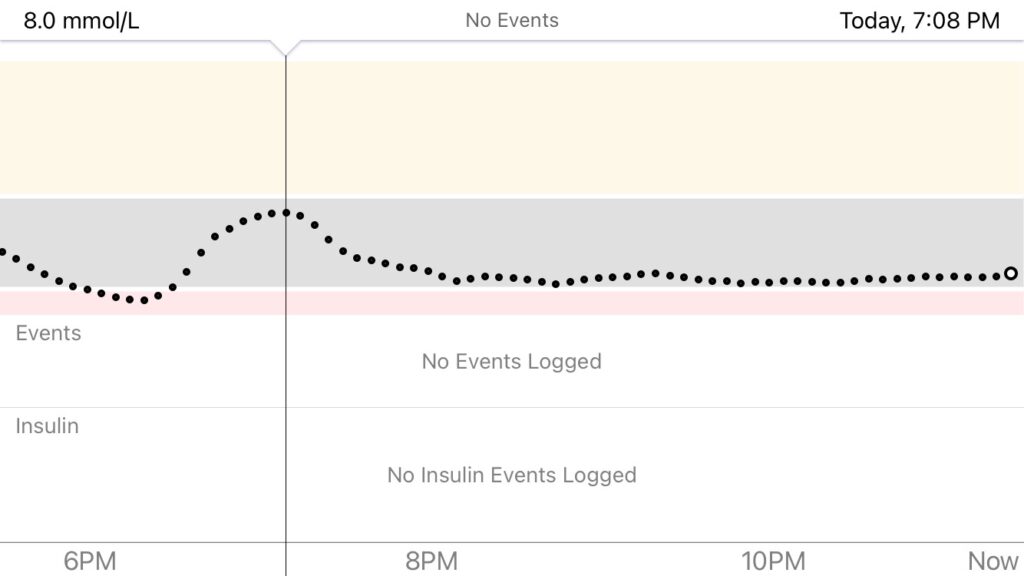
As I finalized this blog post, I thought I should probably add another example to show how this works at the other end of the meal scale, meaning one that is very carb-heavy and includes an unplanned addition of extra carbs (chocolate). So here’s a different recent supper: a baked falafel-ish chickpea cake (many carbs, much fibre), served on white flour flatbread (many, many carbs), with a cucumber-radish salad, a dollop of greek yogurt, and homemade gingersnaps (yet more carbs). After supper, I decided to make whole wheat banana chocolate chip muffins for my kids, during the baking of which I snacked on 20 grams of semisweet chocolate chips and 10 grams of pumpkin seeds (about 12g more carbs, plus extra fat), adding a layer of complexity to my supper boluses.
The food:
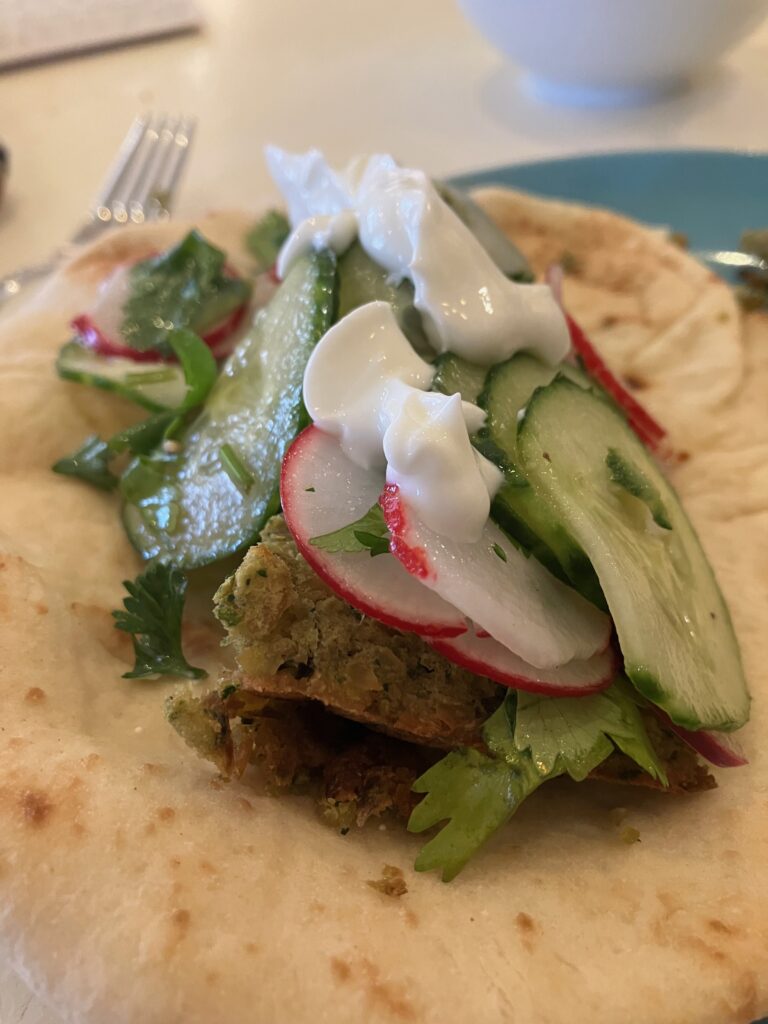
The meal analysis:
The boluses:
- 12 minutes before eating: bolus 88g carbs, which was the carb count pre-chocolate chips (3h absorption in Loop)
- An hour later: bolus 8g carbs for protein (3h absorption in Loop)
- An hour and a half later: eat 20g chocolate chips and 10g pumpkin seeds (+12g carbs, +11g fat, +4g protein), bump up carb bolus to 100g, recalculate fat bolus, don’t worry about minor adjustment to protein
- 3 hours later: bolus 23 carbs for fat (4h absorption in Loop)
And here’s how it worked out. I rode slightly higher than I might have without the spontaneous chocolate chips but it was fine overall.
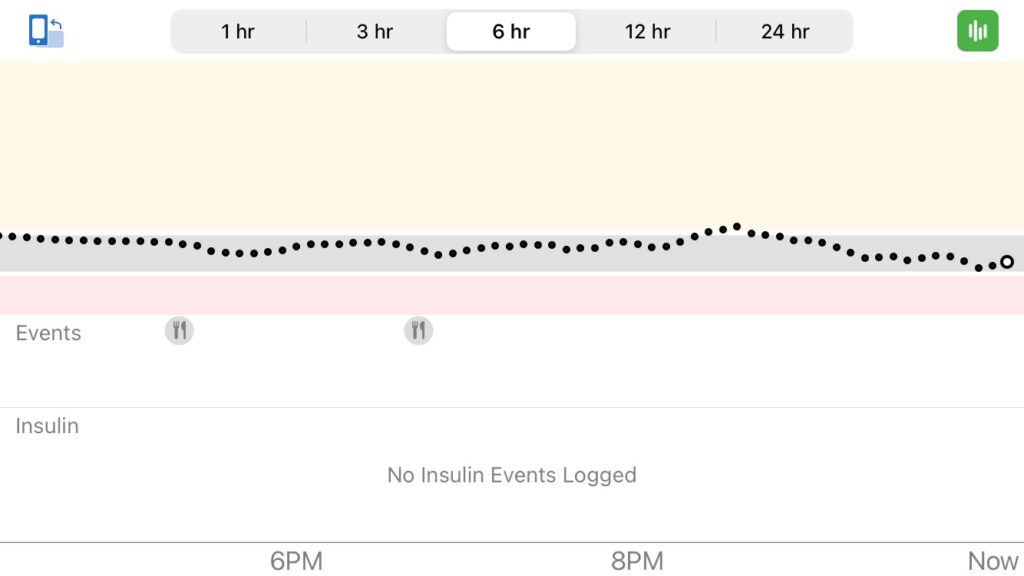
Before looping, I used extended boluses all the time to account for fat and protein. I’ve been on a pump for 20+ years so I didn’t know enough to even consider this on multiple daily injections (MDI), but the Juicebox podcast (see section: Podcasts) once had an episode with a woman on MDI who had a fascinating idea to mix rapid acting insulin (e.g., Humalog, NovoRapid, or Fiasp) with Regular insulin for protein- or fat-heavy meals, eliminating the need for a second injection later. I thought that was absolutely brilliant and will definitely try that if I am ever back on MDI.
Repeated Foods
Shorter version: Like most people, I have favourite meals. It has been helpful to me to incorporate T1D considerations into the selection of what gets to be a favourite. (next section)
Longer version: It was worth my time to find a few meals that are predictable in the way my body responds to them, that I like, and that are often available. When needed, I can use these on repeat. My top one of these is plain greek yogurt with nuts, seeds, bran buds, and some fruit, often a handful of blueberries, which are easy and tasty. It’s delicious, high protein, high fibre, and I know exactly how my body reacts. When I travel for work, I often bring a little bag of nuts and seeds and get some yogurt and fruit once I arrive. If I’m not leaving the country and therefore don’t have to go through border control, I bring the yogurt and fruit with me. Blueberries travel well when they are already mixed into the yogurt. During a time with (too) much travel, a security agent once greeted me at the Quebec City airport as, “la madame avec le yogourt!” (“Hey, it’s the lady with the yogurt!”) I also use the predictability of this yogurt concoction sometimes if I’m having a really rollercoaster-y day and need to reset.
My favourite foods that work great for my T1D are:
Breakfast
- before a run if I’m in a rush and want some food but not too much: a bit of protein powder and milk, or half a banana with a spoonful of peanut butter
- cold weather: oatmeal (takes a longer prebolus than most foods), whole wheat raisin bread toast with peanut butter and banana
- warm weather: plain Greek yogurt with nuts, seeds, bran buds, and berries or chopped fruit on top (can also be used for snacks or other meals while traveling)
Snacks
- a banana and a scoop of peanut butter on a plate (I dip the banana in the peanut butter)
- a handful of cherry tomatoes
- a fried egg on some greens (whatever I have on hand, often spinach … the runny yolk on the greens is so good)
- an egg puck (what my kids call little mini-quiches I make and put in the freezer for breakfasts and snacks: 6 eggs and a variety of chopped vegetables & herbs baked in 12 muffin cups at 325F for half an hour)
- any of my breakfast options (many of these snacks can also sub as quick breakfasts)
- baked goods if we have them (e.g., I’m especially fond of these lemon blueberry oat cakes)
- celery, toast, or an apple + peanut butter or other nut butter
- cereal (cereal is such a comfort food for me—when I was a kid, there were times when my little sister and I ate it for every meal—and I don’t love bolusing for it in the morning, so I make it work for me as an occasional snack)
- cheese + ____ (crackers, vegetable sticks, a sliced apple or pear, you name it …)
- chocolate (not so much a snack as a treat …)
- hard-boiled eggs (I love a hard boiled egg with a sliced tomato, with salt and pepper on both)
- kefir, plain Greek yogurt, milk, or water + protein powder
- mixed plain Greek yogurt & cappuccino-flavoured yogurt with bran buds and chia seeds sprinkled on top
- nuts (walnuts, pecans, almonds, and cashews are my favourites, but I only like cashews roasted with salt, so I favour the first three for healthy snacking)
- seeds (especially toasted pumpkin seeds)
- popcorn with salt and nutritional yeast (the latter because that’s what they did at the commune where my husband grew up … it’s delicious and adds B vitamins, which can be harder to get if you don’t eat a lot of meat)
Lunch
- any weather: an egg or two plus extra egg whites with vegetables mixed in (green onions, peppers, mushrooms, spinach, whatever we have on hand) scrambled or cooked as an omelet + whole wheat toast
- cold weather: leftover soups and stews from suppers (typically kept in the fridge as planned leftovers but I also freeze single servings in these cubes to have backups in the freezer for busy weeks)
- warm weather: bean salads (I love this recipe and make variations on it with white beans or chickpeas nearly every week all summer); plain Greek yogurt with fruit, nuts & seeds; fruit smoothies with protein powder
Supper varies a lot. It’s really important to me to have family suppers, as I didn’t have that consistently as a child. It also fits with my life because I enjoy cooking and find it a relaxing break from other responsibilities. I often listen to podcasts while chopping things, and it’s a nice contrast from work time, where I am thinking hard and juggling grants, papers, students, reviews, budgets, service commitments, meetings, etc.
I plan suppers for the week around our schedules and the weather. My husband and I were both vegetarian for a long time. We started eating some meat again when I was struggling to keep my iron levels up pre-pregnancy, but we still prefer to have mostly legume-based meals for taste, cost, and environmental reasons. We try to have fish once or twice a week (with at least one of those being oily fish) and meat twice a month. I listed some family favourites for my dad recently, because he wants to eat more beans and pulses, and my eldest kid also wants to have these while nearing independence. I posted them plus a few other favourites as well for anyone looking for new ideas:
- bean chili
- black bean tacos
- black bean & corn tacos
- black bean & tomato quinoa salad with lime
- black bean, sweet potato, and peanut stew
- black bean soup & alsacienne whole wheat biscuits
- cassoulet
- canned fish (tuna, mackerel, sardines) cakes on greens
- corn fritters on greens
- curried vegetable and chickpea stew on couscous
- falafel-inspired baked cake & flatbread of some kind (the cake can be made ahead, frozen, then thawed and baked in any lightly oiled pan)
- fish amandine
- fish in packets
- fish with mustard-maple glaze (good salmon is hard/expensive to get here, so I just substitute other fish and otherwise make this as written)
- green lentil salad with flatbread
- green lentil soup with tofu (a new favourite this year, though my youngest is not such a fan)
- lentil chard soup & alsacienne whole wheat biscuits
- lentil spinach dhal (this dehydrates wonderfully for backpacking)
- lentilles du puy green soup made with goat cheese instead of feta (this reheats surprisingly well)
- mac & cheese, slightly healthified
- red lentil fritters on greens (I recommend mixing flour or other binding agent right into the batter so they aren’t so drippy)
- roasted cauliflower soup
- roasted sweet potato & ginger soup served with a dollop of plain yogurt and a generous handful of toasted pumpkin seeds
- stuffed cabbage soup made with diced tomatoes instead of sauce and an alternative to ground beef
- sweet potatoes with warm black bean salad with garlic added to the salad and served with greek yogurt mixed with lime juice
- white bean, barley & greens stew
We almost always have dessert. It is often two homemade cookies per person (about the equivalent of one medium-sized store-bought cookie) and fruit. I love making fruit plates and bowls, because I love fruit and I find that my kids (and everyone else, for that matter, including myself) eat a wide range of fruit enthusiastically when it is cut up and presented to them, whereas they don’t get as much variety when they fetch it for themselves one piece at a time.
Rollercoaster, Get Off The
Shorter version: It is worth my effort to get off a BG rollercoaster as soon as possible. This often requires avoiding tricky foods until I am level again. (next section)
Longer version: Sometimes, I have a high or low that starts a rollercoaster. I have learned through those experiences and different ways I dealt with them that it’s usually worth my effort to get off the rollercoaster as soon as possible. Typically, my best way to do this is to avoid eating or to eat slow, predictable foods until I level out and can start fresh. (My go-to for this is plain greek yogurt with some sort of fruit, often a handful of blueberries, and a mix of seeds, nuts, and a bit of bran cereal.)
Taking the time to level out can be tough to make myself do, usually because the rollercoaster makes me feel so exhausted that I really don’t want to do anything that requires effort. But when I exert the effort, it’s worth it.
After I’ve leveled out, if I can, I try to avoid anything too unpredictable for another 24 hours or so. This is because I find that, after a tough low/high I’m more prone to a second (or third or fourth …) one. This is issue with lows is known, but I have not seen science on the same issue with highs. I suspect the issue is that there is something underlying the first high that has not disappeared (for example, hormones.)
Routines & Rituals
Shorter version: I have found it useful to set alarms and build semi-pleasant rituals and ways of thinking around the things I know I should do for my T1D. (next section)
Longer version: There are some T1D tasks that I just find tedious and/or difficult to remember. The best thing I learned to do to address my dislike was building a little almost-pleasant ritual around each of these tasks.
One of the best things I ever did when I was exhausted by young children and too often forgot to get my insulin moving well ahead of supper was to set daily vibrate-only alarms on my phone half an hour before I typically eat. This might not have worked as well during times in my life when I had a less regular schedule, but these days, it is a great way to quickly remind myself to take a minute and think about what T1D needs in that moment. To make this almost-pleasant, I label the alarms, “supper soon with [family initials].” I do the same thing to remind myself to consider an override/temp basal in advance of bedtime yoga with my eldest, “yoga with [16-year-old’s name]? set override.”
For set changes, I grab my headphones, put on something I like to listen to (often a podcast, sometimes music), alert my family that I’m changing my set so please don’t interrupt me, lock the door, and change my set. I alert my family and lock the door because I realized at one point that what I hated most about set changes was being interrupted and occasionally startled while I’m pushing a large needle into my body. (I suspect this is because I was visiting my mom the first time I had to change a set. She made gasping noises as I put the needle in, as though she was the one experiencing pain. It was a bad experience when I was already nervous, and it set a really bad tone for me for subsequent set changes.)
For putting cream on my feet, I started seeing it as taking care of myself rather than something tiresome I had to do. That shifted my perspective and therefore my attitude about the task. I am still not perfect about this, but I am much better than I used to be. My endo was really happy the last time she checked my feet.
I’ve also never been very fond of flossing my teeth. It helped me to apply some of those same routine/ritual ideas to flossing, which had benefits beyond just my teeth. There are known links between oral health and cardiovascular health, so it’s a good idea to do this anyway. But there’s also a larger benefit. It makes me feel good about taking care of myself to do something I don’t love doing, which helps me feel more motivated to take care of myself in other ways. I am a, “success breeds success,” person, meaning I do better when I feel like I’m not a failure. Flossing makes me feel like a success at self-care. When I do it before bed, it helps me feel like the next day is more likely to be a good one.
Science & Research
Shorter version: In my view, T1D research is getting better, partly because of changes in the scientific culture. I do not expect to see a complete, lasting, biological cure in my lifetime, but I would be delighted to be surprised. I do think it’s a promising time for those who are newly diagnosed or close to being diagnosed, and this is one of the reasons my kids participated in TrialNet. For myself, I would love to see things like glucose-responsive insulin (a.k.a. “smart” insulin) in my lifetime. Taking a shot once or twice a day and never needing to worry about my BGs would be a huge reduction in the effort I have to put into T1D management. As a scientist, I am acutely aware that research questions addressed in papers are rarely the questions I have about my individual care, so I try not to torture myself by reading too many of those papers. (next section)
Longer version: Although I am a scientist, I didn’t set out to do research in diabetes. (I do currently do some work in this area, and have been expanding my research interests in T1D of late.) I had a question about this recently when I was giving a guest lecture in a colleague’s course, and my answer was that as a woman in engineering, I already had to work harder to be taken seriously, and, back when I was more junior, expertise from lived experience was rarely well-respected in most health research. I didn’t want to fight multiple battles at once to establish credibility. (Side note: I know multiple senior male scientists who are both working in and living with T1D, but I’ve never met a woman more senior than I am in that situation. If you are out there, fellow full prof with T1D, hit me up if you see this post!) I think science and research cultures are improving, so in the years to come, I hope to see more research about T1D led by people living with T1D. Some of the positive changes include involving people living with the condition as members of research teams, creating consortia that enable higher-quality studies, and sharing data and research more openly.
I still don’t follow cure research extremely closely. It isn’t my field, and it’s just too frustrating sometimes to deal with the hype. I do not count on seeing a cure in my lifetime, but my life has been improved over the years by new technology, and that’s been pretty great. I think there are a number of interesting avenues at the moment. It’s an exciting time in T1D research. I don’t expect to personally benefit from some of the ideas in the pipeline (e.g., immunotherapy) but I’d love to be surprised. If glucose-responsive insulin comes to fruition and is accessible (read: not prohibitively expensive), that would be very close to a cure as far as I’m concerned. Being able to simply take one or two shots a day and trust that the insulin will only act when needed would be a huge reduction in the work I have to do in my daily balancing act. In the meantime, I’ve always tried to participate in research when it made sense for me, including research involving my family. These include:
- My eldest was enrolled in a trial at birth for infants of parents with T1D (it was called TRIGR and is now done) and both my kids were screened for TrialNet.
- I am enrolled in a registry called BETTER that has been running in Quebec (where I live) for some time and is now available across Canada. (BETTER is sort of the Canadian version of the US registry T1D Exchange.)
Side note: If you live in Canada and are interested in participating in research (meaning your answers/data get used in studies), you may want to create an account at ConnecT1D and find out what studies are available that might be of interest to you. If you are interested in partnering with research teams (meaning you help determine what questions get asked and how studies are run) you may want to check out Diabetes Action Canada. (Disclosure: I am not involved in running ConnecT1D but I am involved in Diabetes Action Canada, which created ConnecT1D.)
One thing I always keep in mind as a scientist is that, while it’s useful to be aware of research findings, the research questions addressed in many studies often differ from my questions for my own care. The biggest difference is that most trials these days are analyzed using intention-to-treat analyses; whereas I want per-protocol answers. In plain English, whereas a randomized controlled trial of T1D devices might answer the question, “What happens if we give people with T1D access to a complex device, regardless of how they use it in their lives?” I want to know, “What will my results be with that device in my life, knowing that I will bring my type A personality to the table?” If I were running a health system, I would want the answer to the first question. But as a human individual with T1D, I want the answer to the second question. I would love it if more authors and journals would provide per-protocol analyses in the supplementary materials. (And report summary statistics by sex/gender, age, ethnocultural group, socioeconomic status, etc., too.)
Settings, Having A Record Of
Shorter version: It has been useful to me to have a record of my settings, be it paper or electronic, separate from the device using the settings. This typically looks like a written record on a piece of paper, photos of pump screens, or screenshots from my current system. (next section)
Longer version: I’ve used a pump for 20+ years and an automated insulin delivery system for 4 years. I tweak my settings as needed. Over the years, I learned to keep either a written paper copy of my settings in my “just in case” daily kit, or photos or screenshots of settings on my phone. Sometimes that looked like photos of my pump screens; now it is screenshots of different setting screens, filed in folders named for each screen. Having those records to hand has saved me, for example, when my pump crashed at my sister’s wedding on a long weekend in a rural area and I needed to figure out how to revert back to multiple daily injections using whatever insulin I could get at the nearest small town pharmacy.
(For more on settings, see the formulae from Think Like A Pancreas in the section Insulin.)
Sleep
Shorter version: T1D can really interfere with sleep, making T1D harder to manage. It is a difficult cycle. I find it useful to keep low treatments, etc. within reach while I am sleeping, to avoid eating before bed, and to prioritize sleep as much as I can within the constraints of my life. (next section)
Longer version: The relationship between T1D and sleep is a frustrating cycle. When I get poor sleep, my T1D is harder to manage, which means my sleep is more likely to be disrupted. The older I get, the less well I deal with T1D sleep disruptions, too. I honestly wonder what proportion of the longer-term negative effects of diabetes are actually due to decades of disrupted sleep.
My best lesson for good sleep is that looping has been transformative (see more in section Looping.) I have slept better since I started looping than in the many decades previously. But otherwise, one of the best habits I ever developed was making sure I have my CGM reader/phone, meter, hypo treatment, and some water within reach while I’m sleeping. I am not 100% perfect at this habit at home, but it’s a strict rule when I’m traveling alone for work, even though I am now less likely to need it. If I do go low at night, everything I need is right there.
Another useful lesson is that I sleep better if I don’t eat too close to bedtime. This was a very hard lesson to learn, because I grew up during the time when a bedtime snack was essential to absorb the peak of NPH insulin given before supper. As a kid, I frequently had severe lows in the early morning hours that required glucagon. Even though I always ate my prescribed snack (suggesting that the snack probably wasn’t the problem), it was still hammered into me that my bedtime snack was critical to avoid those lows. In short, I have been deeply conditioned to feel like I am supposed to have a bedtime snack and am somehow wrong and bad if I don’t have one. Also, I like snacks, and it’s a pleasant way to end the day. However, with newer insulins, I don’t need the snack anymore, and avoiding eating after supper removes a lot of variables that go into overnight blood sugar. I’ve learned to forgo a bedtime snack most of the time and have become a fan of afternoon snacks instead. Eating enough during the day is really helpful to me, especially on active days (which is most of them.) I regularly drink decaf or herbal tea before bed while reading. The tea kind of stands in for my old snack and provides that comforting sense of routine and ritual. If I really feel like I need a snack at night, I try to make it a protein snack (e.g., a hard-boiled egg) or small and protein-heavy (e.g., the other night I had a small bowl of some bean salad I’d just made for the week plus a hard-boiled egg.)
Getting decent sleep is really helpful to T1D management. Everything is easier if I’ve slept reasonably well. This is yet another reason to thank the people who developed algorithmic options, and also to thank my children for no longer being in the stage of life in which they frequently need a parent at night.
Support
Shorter version: It’s hard to ask for support because it’s hard to trust people to be reliable. When I’ve found people I can trust, it has been worth it to take the emotional risk of asking. (next section)
Longer version: The more secure I feel, the easier I find it to ask for support. This is frustrating, because when I’m feeling less secure, that’s when I most need support, but it is the reality of my emotions. I try to keep that in mind and make myself ask for what helps me, even if I don’t especially want to ask. I never frame it as asking for what I need, because what helps me rarely rises to the level of need. I am constantly torn between my decades of life lessons that this condition is my responsibility, no one else’s, and my beliefs that it’s worth pursuing a world in which we support each other and seek and provide accommodations. In short, I can usually get by without the support, but it can help, and it may help others in the future, so I have learned to force myself to ask.
The support I have asked for (and received) that has been most helpful to me over the years have been when I asked:
- to take a make-up exam after I was so low that I missed a midterm during my undergrad
- to take exams in a location where they would let me bring my meter and low treatment
- my husband to follow my Dexcom and have a predetermined routine when I am traveling solo for what to do if I am low and not responding
- my in-laws, dad, sister, and sister’s family to help me plan for post-meal exercise by discussing afternoon plans prior to the lunch, and to give me a 20-minute heads up when meals will be served when we are visiting them
- my husband to listen to a diabetes podcast so that he understood a bit more without me having to put more energy into diabetes-related topics by explaining them to him
I have also asked but have often been disappointed in academic spaces when I request that we stick to the posted schedule at a conference, meeting, grant review panel, and so on. They say yes, but then too often fail to do it. (Protip to academics: instead of, “Does anyone mind if we go over?” try, “Sorry, Brett, I’m going to have to cut you off there as we’ve reach the scheduled lunch/break time. Let’s pick this back up when we come back at [time].”) I keep asking and pointing out that this is an accessibility issue. I hope that someday I can trust those yesses.
Technology & Tools
Shorter version: The most helpful modern technologies for me are, in order: an automated insulin delivery system (“closed loop system”), a continuous glucose monitor, an insulin pump, and a nice lancing device. I would really like it if others in my life were aware that many people use smartphones as medical devices. (next section)
Longer version: Technology and tools have vastly improved my life with T1D. Over my 4 decades with this condition, some highlights include my first glucometer, my first meter that took 5 seconds instead of 2+ minutes, human synthetic insulin, insulin pens, and faster insulins.
More recently, newer tech has really revolutionized my life. I once had a mild difference of opinion over aging with someone about my age who does not have T1D. I said that I love aging. They grudgingly commented, “yeah, I guess it’s better than the alternative.” Try as I might, I couldn’t adequately convey that I don’t find it just better than the alternative, I physically feel better in my forties than I did in my twenties.
In retrospect, what I was failing to consider was that people my age with T1D came into middle age right as diabetes technology was leaping forward. Since I’m fortunate to be able to access technology (sometimes with considerable difficulty, but I can usually get it eventually), my forties have been the time when I’ve suddenly been able to sleep through the night, exercise more easily, eat more flexibly, and therefore feel physically better. Perhaps unsurprisingly then, a great lesson for me has been to try any new technology that I can reasonably access.
For me, the most life-changing modern technology these days are, in order of importance:
Automated insulin delivery system. I’m kind of cheating in listing this first, because you can’t have an automated insulin delivery system without having a continuous glucose monitor and pump, the technologies I am listing second and third, respectively. But it’s the honest truth that the automated system has been the most transformative of all the tech I’ve adopted in the past decade or two. See section: Looping for more on this.
Continuous glucose monitor (CGM). If I absolutely had to choose only one thing (meaning I couldn’t cheat by choosing the multi-technology assembly of an automated insulin delivery system), a CGM would be my top choice. Getting my first CGM, a Dexcom 7+ in 2009, was such a positive thing for me. I’d been hypo unaware for years at that point, so just having that extra help to alert me about my lows was huge. As a bonus, it also helped me see patterns after insulin, food, and activity, and I was able to incorporate my knowledge of those patterns into my management. I currently use a Dexcom G6 and have previously used the G4, G5, Medtronic Enlite, and Libre 1. I did not like either the Enlite or the Libre. Neither was accurate for me. They missed lows, which is the most important reason I wear a CGM. I know that others find them extremely accurate, especially the newer versions. I’m glad there are multiple products out there, because I think it helps push the technology forward, and I can imagine that different products may be better for different people with different body chemistry. G6 is extremely accurate for me. I do not calibrate it unless it requests a calibration, which has only ever happened to me once.
Because I was paying out of pocket substantially for a long time, I used to try to stretch out my sensors. I found that having more level BGs made the sensors last longer for me. I could routinely count on 24 accurate days out of a G5 sensor, and sometimes longer. Now that G6 is covered in my province, it means my work insurance has to cover it, so I no longer try to stretch out my sensors, but I still find that my sensors seem more accurate and less jumpy when my BGs are more level. Staying level of day 1 seems to especially help me get bang-on accuracy for the full 10 days.
I’m no longer certain what I think about people without diabetes wearing CGM. I used to strongly dislike it, because in addition to minor annoyances like seeing tech bros believe they’ve invented the glycemic index, there were also genuine concerns about how people with diabetes had trouble accessing CGM, there were sometimes shortages of supplies, and there was never any discussion of prioritizing those using CGM to keep themselves alive over those who don’t truly need CGM. Also, CGMs do produce plastic waste. Now it’s a more mature technology and shortages seem to be less of an issue, but people with diabetes still have massive trouble with access. I would love to believe that with more widespread use, the costs will come down, but I worry that companies will prioritize the larger market of people whose BGs are never going to touch 2.6 or 17.9 mmol/L (47 or 322 mg/dl), making accuracy in the very low and very high ranges, the critical values for those of us whose lives depend on these devices, less important to them. I will acknowledge that one positive thing from non-diabetics using CGM is that I personally find it helpful and fascinating to see graphs from people without T1D, and to read statements from scientists like:
“Summary: In the absence of any evidence to the contrary it’s reasonable to suggest that post-meal excursions into the 9-11mmol/L [162-198 mg/dl] range occurs quite a lot in people with a perfectly fine A1c, and is probably a normal part of human physiology and nothing to worry about.”
I’ve got a CGM – what kinds of values are normal?
(Side note: I don’t really know—this isn’t my area of science—but I do sometimes wonder if brief glucose excursions like those that occur among nondiabetic people might actually be a positive thing for human bodies, in the same way that regular exposure to small, safe amounts of allergens can actually reduce allergies. I’m not personally going to try to have lows or highs on purpose, but I am curious to know whether perfectly flat lines all the time are actually good for human bodies or not.)
I keep my CGM alerts very tight during the day. I move them around sometimes, depending on activity, travel, etc. Most of the time, my low alert is set at 4.2 mmol/L (76 mg/dl) and my high alert is set at the lowest possible level, 6.7 mmol/L (121 mg/dl). I’ve heard that Dexcom presented data at a conference once showing that people with lower high alerts have better BGs. I’d love to see a trial on this that includes measures of alert fatigue, including proxies like how often do people swipe or snooze rather than acknowledging the alert. But for me, at least, the result makes sense. I find that keeping my range tighter makes BG management easier, not harder, because I can address a low or high before it gets out of hand. I end up needing to take less action, not more. I do set all my alerts to vibrate-only wherever possible, and set the snooze to be an hour for low and two hours for high. (I have treated, I am coming up, and I do not need twelve notifications that I am still low, thank you very much, Dexcom.) My current nighttime range is much wider: 3.3-10.0 mmol/L (59-180 mg/dl). This is because I highly value sleep and I trust Loop to handle minor lows and highs on the occasions they occur. I only want to be awoken if it’s really bad. When I travel solo, I set my nighttime low alert higher, turn on audible alerts, and also increase the target on Loop.
I find the best time to have a 2-hour warm-up gap is first thing in the morning. I miss the 7-day sensors because I could always have it on a weekend morning, and could typically arrange my morning such that I just wouldn’t have coffee or food until the sensor was up and running, so nothing much happened with my blood sugar and I could start out nice and level, making for much better sensor accuracy from the get-go. With the 10-day versions, that no longer works quite as well, but I manage it as best as I can. I look forward to potentially seeing a 14-day sensor in the future, and I expect the 30-minute warm-up for the G7 will make this substantially easier.
Insulin pump. My first pump (a Deltec Cozmo in 2003) was just as life-changing as CGM, but now that I have both, if I absolutely had to choose, CGM would get the edge. Still, having a pump has been incredibly useful to me. Being able to fine-tune my basal pattern has been so helpful, and being able to give tiny amounts of insulin very precisely is really helpful when your body responds to small amounts of insulin, as mine does. I also love being able to reduce my basal to head off lows. My favourite feature on the Cozmo was being able to pre-program temporary basals of 0 units per hour for 30, 45, 60, and 90 minutes. I had those set up so that I could turn them on with just a few button presses. I used that feature all the time. I also like being on a pump because I can reduce my basal in advance of physical activity, helping to keep me from going low during said activity.
I will also add here that I am very impressed by the engineering in Medtronic pumps. I am currently using an ooooold Medtronic pump (I have a 722 and a 522 as backup) as part of my do-it-myself artificial pancreas system and wow, they just keep on ticking. (Dear Medtronic: if you make future pumps plug & play like you announced at a conference some years ago, people like me will buy them.)
Delica lancing device. Many years ago, the One Touch meter that came with one of my early pumps (I think it was my first Animas pump) came with a Delica lancing device. I’ve long since moved on from that pump and meter, but I still use the same lancing device. I was never particularly bothered by the more painful lancets, but it has been nice to have an easier option.
I will note that my top technologies above run on my phone. This is great most of the time, because I always have my phone with me. But it does cause some problems in my life, because many people are unaware that many others use smartphones as medical devices. For example, in addition to my own use, I know that others use their smartphone to control their hearing aids, as communication aids, etc. This lack of awareness would not be a huge problem if it weren’t for the assumption that no one needs to have their phone with them, but that assumption is widespread and creates problems. This has impacted me in ways ranging from side-eye from colleagues when I am using my phone in a meeting to hurtful comments from family (“we don’t allow phones at the table,”) to outright barriers. Not long ago, after being accepted to participate in a ‘Science Meets Parliament’ program whose in-person component was delayed due to Covid-19, I ultimately declined to participate in the in-person component because, among other reasons, I was worried about the ‘no phone’ rule at one of the event locations. They said they would help figure something out, but there were no guarantees. I know that, too often, these rules are inflexible and any workaround involves me being made to feel like a problematic burden due to my accessibility need. I just didn’t have the energy for that uncertainty and those feelings at that time.
Travel
Shorter version: I find it useful to have a checklist of T1D supplies, keep supplies with me, avoid high carb/fat meals when traveling solo, and plan to use about 20% more insulin on travel days. (next section)
Longer version: Pre-pandemic, I traveled a fair amount for work, and sometimes to see family. Some things I learned to make travel easier for me:
- keep a checklist of supplies to make packing easier
- bring lots of backup supplies, but also remember that if I am caught out, I will handle it somehow
- diabetic supplies go in carry-on, not checked luggage (I typically travel carry-on only, anyway)
- traveling solo is not the time for me to try exciting new food, but if I’m going to try something, try something that is lower in both carbs and fat
- keep low kit (glucose tabs, gel, test kit) within reach when sleeping
- sedentary travel days (i.e., days with minimal exercise because I am mostly in a car, on a train, or on a plane) seem to work best with a 120% override (i.e., 20% more insulin than usual)
- have a checklist on my phone, the fridge, or the front door with a list of last-minute don’t forget things, like grabbing my extra insulin out of the fridge
- wrap a spare transmitter around a sensor using a couple of elastics (saves space and keeps them together)
Water
Shorter version: Drinking plenty of water (2-3 L per day) makes T1D management easier for me. (next section)
Longer version: Water makes everything work better for me. (I am talking about drinking it here, though swimming in it is also fantastic.) Things that I notice when I drink plenty of water:
- continuous glucose sensors work better
- insulin works faster
- hypos resolve faster
- I feel more energetic
I find it useful to drink about 500mL (2 cups) first thing in the morning and to aim for at least 2-3 L (8-12 cups) per day. I have a bunch of 1 L Nalgene bottles that we take camping, and I just refill from the tap as needed, thanking my lucky stars I live in a place with good, safe tap water. This has not always been the case, so I really appreciate it.
Weighing Food
Shorter version: It’s been worth my time to develop a habit of weighing food. Accurate boluses make post-meal time more relaxing. (next section)
Longer version: I weigh a lot of my food. I used to think it was a pain, but it’s one of those things that got really easy when I started just doing it routinely. It makes it easier to bolus correctly for higher-carb foods (e.g., bananas, oatmeal, potatoes) and higher-fat foods (e.g., nuts, seeds, cheese.) When I can bolus more accurately, the likelihood of post-meal problems goes down, so I can just get on with my life, knowing that my BGs are doing well.
Below is a photo of the scale I use. I got it from Lee Valley Tools for less than $20 Canadian or less than $15 US. I also have a little travel scale that I got elsewhere that I’m pretty sure is designed for, uh, things other than food. That smaller “travel” scale is ok for small amounts, but I don’t love it. The Lee Valley scale is not marketed as a travel scale but it is small enough that if I have space in my bag, I typically pop it in its box and take it with me.
Weight Management
Shorter version: Weight is really personal. T1D adds levels of difficulty. In my view, people should be supported in deciding for themselves how and whether to manage their weight. A while back, I wanted to lose weight (alongside increasing strength) so I could more easily go from running 3 times a week to 5-6 times a week without my knees and hips complaining. So I lost weight and maintained it by a) starting from a place where my BGs were doing well and I was eating enough, b) using a food logging app on my phone, c) cutting calories by 250-500 per day until I had lost 5-10% of body weight, d) maintaining for about 6 months before aiming to drop any more, then e) repeating steps a-d. To make sure I would never hesitate to treat a low but would also be less likely to overtreat, I didn’t count glucose tabs in calorie counts, but I did count any other low treatment. This effort was worth it: I now happily run 5-6 times a week, and it is really helpful for my mental health. (next section)
Caveats: Weight is a fraught issue for a lot of people, and T1D adds many complicating layers. There’s a lot more to health than body weight. I know plenty of people who are heavier and healthy, as well as people who are lighter and unhealthy. Even health can be a fraught issue. Not everyone has the same values, nor do we all have the same opportunities, and I am very troubled by messaging that implies (or straight-out says) that healthier people are better people. I don’t agree with that idea. I think everyone should make their own decisions about health and weight, ideally with a range of reasonable options available to them in their life and genuine support from knowledgeable health professionals. No one should ever feel pressured (directly or indirectly) to change their body shape. This is my own experience, based on what matters to me in my life.
Longer version: I dropped a fair amount of weight a while back. (Numbers: I’m 172 cm/5’8”, and I went from 81 kg/178 lbs to 64 kg/141 lbs over four years, with stretches of time in active weight loss mode, and stretches of time in ‘let’s take a break and maintain for a while’ mode. I’ve kept it off since.) I decided to reduce my weight because I was running 3 times a week, it was so helpful to my mental health and overall well-being, and I wanted to be able to run 5-6 days a week long term. My dad runs regularly at age 75, and I would love to be able to be as active and happy as he is at his age. (He has a small group of 75+ running buddies who set goals like beating last year’s number of runs up a local mountain. They did it!) When I tried running more and longer, I started to notice joint complaints, and I believed I would be less likely to have joint problems or injuries if my body was both lighter (requiring some weight loss) and stronger (requiring more strength training.) I also wanted to be able to keep doing other things I enjoy, like hiking and canoeing trips. Logging more kilometres running helps me be in spontaneous-trip-ready shape. Finally, I knew that losing weight gets harder as one gets older, so if I was ever going to do it, it would be better to do it sooner than later.
I’d lost weight before for specific purposes, namely, after having my babies, and while training for sports nationals the same year I got married. I’ve always found that weight management works very similarly to blood glucose management: it really benefits from steadiness and consistency. Perfectionism hurts rather than helps, and there will always be bumps in the road, so it’s best to find a sustainable approach that I can maintain indefinitely. I also find weight loss easier when my T1D is well-managed, because I’m not chasing lows and dealing with the physical effects of highs and lows, so bringing the same steady, resilient attitude to both is helpful.
The same approach has always worked for me: start from a place where my BGs are pretty good and I know I’m eating enough (typically at least 2000-2600 calories/day, depending on activity levels), then run a small (250-500 calories/day) caloric deficit overall, do it consistently for an extended period of time, then slowly ramp that 250-500 deficit back to up to balanced. It is not fast, but it is effective for me. I also understand that, to avoid too much metabolic adaptation (i.e., having your body fight back against the weight loss) it is best to lose a maximum of 5-10% of body weight, then take a break and hold steady for at least six months before going further. I did not do that exactly to the letter, but that’s close to what I ended up doing.
I’ve never personally lost weight using specific eating plans. I tried low carb nearly 20 years ago, the year I was getting married, in an attempt to improve both weight and blood sugar management. It was a disaster for me in both respects. I worked really hard for 5 months, following instructions to the letter, but my blood sugars became way less stable, and I gained weight. According to a scientist I know, although many people lose weight eating low carb and find blood sugars easier to manage, some people have this paradoxical effect. It’s possible that was the case for me. It’s also extremely possible that receiving the guidance that I could eat as much cheese, nuts, and seeds as I wanted was an easy, delicious route to thousands of calories a day. (I really, really like those foods.)
To run a caloric deficit, I set a weight-based calorie limit in the food tracking app I was already using to more accurately count carbs. I set it so that it cut either 250 or 500 calories per day. I could still eat whatever I want, as long as it was within calorie limits. This meant that I was more likely to choose foods that were highly satieting. Most often that meant high fibre and high protein. Sometimes it meant an ice cream bar. The one T1D-relevant thing I worried about is that I know myself and my hit-my-targets, achievement-oriented mindset. I worried that by setting a calorie limit, I would be tempted to delay or avoid treating hypos because it would mess up my day/streak in the app. So I decided I would not count glucose tabs in my calories, but I would count any other hypo treatment. This isn’t entirely accurate. A glucose tab has 15 calories, not zero. But, because I don’t like them, I have almost never eaten more glucose tabs than I need and I rarely need more than 1-3 tablets, so at most, this is an undercount of 15-45 calories, which is an acceptable margin of error for me. It makes it so that I don’t hesitate to treat a low, and I’m more likely to treat with the most effective, fastest treatment for me.
As I lost weight, I knew I would need to adjust my settings. I was already pretty comfortable doing that, but it was still helpful to refer to the formulas in Think Like A Pancreas by Gary Scheiner (see the formulae in section: Insulin) to help me structure my thinking. Of course, it would be great to go over the fine details of my settings with a health professional, but that is not always realistic for me, and I’ve had so many years now that I am very confident adjusting my own settings. My endo is also comfortable with me doing that, but even if she weren’t, I would probably still do it, just less openly.
During this time, I was really careful about my risk of falling into disordered eating again. I had disordered eating in my teens in response to hypos and an unstable home life. I was so anxious about lows and especially being alone during scary lows that I’d often end up substantially overtreating them (the classic, “eat the kitchen,” response), and then once my sugar came back up, I wished I hadn’t gotten so desperate, but didn’t want to go low again so was scared to give a large dose of insulin to cover the overtreatment. I would also occasionally pre-overtreat to avoid a low later. I always felt very comforted by having lots of carbs on board, because then I felt safely above the BG danger zone. Sometimes I also ate more of something just because it was available now, and, due to instability at home, probably wouldn’t be available later. Compounding all this, despite the fact that I was an active, sports-playing teen, I felt guilty about eating a perfectly reasonable amount of calories and having a normal, athletic body (thanks, 80s and 90s media), so I believed I was failing at performing femininity to the expected standard. (I would not have been able to put that into those words at the time, but it’s so clear when I look back. It did not help that I compared myself to my non-T1D sister, who was always thin despite her impressive teen appetite, nor that our mom highly prized physical appearance and struggled a lot with her own weight. She was athletic when she was younger but started gaining weight in her late twenties. It was always very evident she was unhappy about it.) As I had more autonomy over my life in my twenties, all of my negative tendencies decreased. Once I really got a handle on my T1D as a young adult, my “eat the kitchen” lows became thankfully rare events, and as I got older and further away from my childhood environment, I was able to develop a less problematic view of food and my body. All this to say that, like many people, I come at issues around food and weight with a lot of baggage.
I was not able to ditch my baggage by adopting an intuitive eating approach. It just doesn’t work well with my T1D. I really like the idea in principle, but perhaps because I grew up in the days of strict T1D diets, I don’t have a real sense of hunger that I can trust. I do feel a sensation that I call hunger, but it doesn’t always mean the same thing. Sometimes it means I haven’t eaten in 3-6 hours and am actually hungry, sometimes it means that I am crashing low with no warning, and sometimes it mean my BGs are high. I get that feeling around 8-11 mmol/L or 144-198 mg/dl, even if I’ve just eaten, which, frankly, is extra motivation for me to avoid going above 8. I’ve spent a fair amount of effort paying attention to this, and those three very different situations still all feel exactly the same to me. (Side note: I’ve wondered if experiencing 8-11 mmol/L as hunger may be rooted in my teenaged experiences and is therefore more psychological, or if there’s a physiological component and perhaps that’s part of the type 2 cycle, with higher BGs creating a feeling of wanting to eat more, leading to weight gain.) Also, because I have to bolus insulin according to what I eat, and because my insulin needs are relatively low, small differences in the amount of insulin can make a big difference for me. When I bolus more precisely, my BGs are more level and I feel better. Bolusing precisely requires paying attention to what I eat in a way that is at odds with intuitive eating approaches. I am extremely aware of my risk of falling into disordered eating, so I’m careful to avoid that while also being honest with myself that a loosely structured approach seems to work really well for me in many domains, including this one.
Zealots
Shorter version: Zealots in the T1D community are unpleasant, but they are not the majority. My best approach for dealing with them is to be happy for them and move on. (next section)
Longer version: There are zealots in the T1D community. I’ve interacted with them. It is rarely pleasant. There are many people who just want to share what works for them. In my view, this is fine, and I appreciate the chance to learn from others. (That is what I am trying to do here. Please feel free to take and share what works for you and leave the rest.) But then there are the zealots who are convinced that what works for them is best for everyone. In my view, this is not ok. The approach I’ve found most useful in those interactions is, “Wow, that’s great. It sounds like that works really well for you. I’m sincerely happy for you.” Then I exit the conversation as swiftly as possible.
Thank you
Thank you to everyone who made it all the way to the end. I hope some of this was useful to you. I am wishing everyone with T1D as easy a time as possible living with this condition. T1D management has come a long way, and so have we.